NEW DRUGS, POORLY RECOGNISED CONDITIONS, GENETIC POLYMORPHISM AND THE CRISIS IN MENTAL HEALTH
Yolande Lucire PhD MB BS DPM FRANZCP.
WARNING!
Withdrawal
can often be more dangerous than continuing on a medication. It
is important to withdraw extremely slowly from these drugs, usually
over a period of a year or more, under the supervision of a qualified
specialist. |
If you read this and want get off your medicines, please consult these sites and take the information to your doctor.
http://www.mind.org.uk/Information/Booklets/Making+sense/
Making+sense+of+coming+off+psychiatric+drugs.htm
And
http://psychrights.org/Articles/SSRIDiscontinuationSyndrome.htm
And
http://www.benzo.org.uk/healy.htm
Please note mainstream citation base. Where secondary sources have been
shown in links, the author has checked and re-checked primary sources.
1. The Purpose of the Publication.
This paper seeks to inform Australian health professionals, health
administrators, prescribers and citizens that what they have been told
the pharmaceutical industry about a whole new generation of 'serotonin'
drugs is simply not true. The pharmaceutical industry is a client of
the United States Food and Drug Administration, (US FDA) the
Therapeutic goods Administration, (TGA). All have been victims of
corporate fraud which is coming to light now in the United States as a
consequence of litigation by 42 state Attorneys General acting on
behalf of the people.
2. SEROTONIN
From Wikipedia: In the central nervous system,
serotonin is believed to play an important role as a neurotransmitter,
in the inhibition of anger, aggression, body temperature, mood, sleep,
vomiting, sexuality, and appetite. In addition, serotonin is also a
peripheral signal mediator. For instance, serotonin is found
extensively in the human gastrointestinal tract (about 90%), and the
major storage place is platelets in the blood stream.
Drugs to manage serotonin are prescribed on the assumption that
serotonin affects mood and boosts confidence; therefore serotonin must
be in deficit in the depressed. This is about as logical as the
argument that aspirin cures some headaches so headache must be caused
by a deficit of aspirin.
http://www.springerlink.com/content/u37j12152n826q60/fulltext.pdf
But there is no evidence that serotonin is abnormal in depression, and
no scientific basis for the chemical imbalance theory that you will
find on each drug manufacturer's website. We have beyondblue
which, until recently promoted Serotonin theory, and provided general
practitioners with eduction about identifying and treating depression.
http://www.beyondblue.org.au/index.aspx?link_id=&gclid=COCXyqDn9JECFSOYiQod9TdRqQ
The campaign to prevent depression has been so successful that we
currently have a million Australians on antidepressants. And maybe two
million who have tried them. That is one in every five Australians, and
32,000,000 Americans. These drugs make some users fat and
somewhere between 6 and 14% diabetic, depending on which trial you
believe.
http://www.newscientist.com/channel/opinion/mg19726465.700-comment-the-pills-that-make-us-fat.html
3. Australia has NO EFFECTIVE system to alert doctors to problems with new drugs as they Arise.
Weekly alerts are available even for Australian doctors from the US FDA
and they are free. Some changes never filter through to
Australian doctors and when they do it is because a news program on
television has drawn attention to them.
The US FDA was reconsidering its licensing of Chantix, an antismoking
remedy which causes violence and suicidality, just as it was being put
on the Pharmaceutical benefits scheme in Australia. For example, US
doctors get this information:
Audience: Neuropsychiatric and other healthcare professionals, consumers
[Posted 02/01/2008] FDA informed healthcare professionals and
consumers of important revisions to the WARNINGS and PRECAUTIONS
sections of the prescribing information for Chantix regarding serious
neuropsychiatric symptoms experienced in patients taking Chantix. These
symptoms include changes in behavior, agitation, depressed mood,
suicidal ideation, and attempted and completed suicide. While some
patients may have experienced these types of symptoms and events as a
result of nicotine withdrawal, some patients taking Chantix who
experienced serious neuropsychiatric symptoms and events had not yet
discontinued smoking. In most cases, neuropsychiatric symptoms
developed during Chantix treatment, but in others, symptoms developed
following withdrawal of Chantix therapy. See the FDA Information for
Healthcare Professionals Sheet for recommendations and considerations
for healthcare professionals on using Chantix therapy for patients.
[February 01, 2008 - Public Health Advisory - FDA]
[February 01, 2008 - Prescribing Information - Pfizer]
[February 01, 2008 - Healthcare Professional Information Sheet - FDA]
and
http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/psn/transcript.cfm?show=74#3
No alerts went out to emergency rooms to seek this cause for suicide attempts.
Even after the Sunday program has drawn attention to toxic drugs, the
authorities are slow to respond and as with the recent warnings on
Stilnox, advisories sent out by Sanofi Aventis were entirely
inadequate.
We doctors in Australia are not provided with letters, emails or warnings about interactions.
There is little demand in Australia for doctors, especially
psychiatrists, to get informed consent before prescribing. If there
were, it would force doctors to read product information and not to
rely on what drug reps tell them or on fatuous advertisements such as
Zyprexa's "Have you made the change yet?"
MIMS Annual is not on every doctor's desk, not even in every psychiatric ward.
As some psychiatric drugs, specifically Zyprexa, were licensed on
six-week trials, information about what is discovered later just does
not filter through. Drugs trialed for six weeks are given for years.
When they are given to bigger populations and or in doctors' surgeries
where many drugs are being co-prescribed, providing up to date and
frequent alerts is a bare minimum requirement of the licensing
authority.
But that requires a measure of political will that seems to be out
of reach for relevant bodies. It is hardly surprising that health
professionals continue to be misinformed by pharmaceutical companies
and receive insufficient scientific advice themselves.
Whereas in the United States, the Food and Drug Administration can
force drug makers to send out 'Dear Health Professional' letters to
inform of changes in knowledge, our own Therapeutic Goods
Administration (TGA) either does not have that power to order it or
lacks the will to use it.
We do not have the Physicians Desk Reference (PDR) or its equivalent
that the UK and US doctors use, or anything like it. This is what every
doctor in the United Kingdom has within reaching distance.
The Physicians' Desk Reference
lists the following adverse reactions (side effects) to antidepressants
among a host of other physical and neuropsychiatric effects: manic
reaction (mania, e.g. kleptomania, pyromania, dipsomania), emotional
lability (or instability), abnormal thinking, alcohol abuse,
hallucinations, hostility, lack of emotion, paranoid reaction, amnesia,
confusion, agitation, delirium, delusions, hysteria, psychosis, sleep
disorders, abnormal dreams, and discontinuation (withdrawal) syndrome.
Adverse reactions are especially likely when starting or discontinuing
the drug, increasing or lowering the dose or when switching from one
SSRI to another SSRI. Adverse reactions are often diagnosed as bipolar
disorder when the symptoms could be entirely iatrogenic (treatment
induced). Withdrawal, especially abrupt withdrawal, from any of these
medications can also cause severe neuropsychiatric and physical
symptoms. It is important to withdraw extremely slowly from these
drugs, usually over a period of a year or more, under the supervision
of a qualified and experienced specialist.
In addition to the adverse reactions listed in the Physicians' Desk
Reference, the FDA published a Public Health Advisory on March 22, 2004
which states (in part): "Anxiety, agitation, panic attacks, insomnia,
irritability, hostility, impulsivity, akathisia (severe restlessness),
hypomania, and mania have been reported in adult and pediatric patients
being treated with antidepressants for major depressive disorder as
well as for other indications, both psychiatric and nonpsychiatric."
In Australia, instead of accurate and up to date information, we seem
to rely, at all levels, on 'opinion leaders' who append their
names to information provided by the pharmaceutical industry, without
undertaking a great deal of independent research.
It is no secret that incentives offered by pharmaceutical companies can
sometimes be hard to resist. The RANZCP at its conference in 2008 faced
some discord concerning the influence of the pharmaceutical industry on
the behaviours and prescribing habits of psychiatrists, but the
industry has prevailed.
A SENIOR
member of the Royal Australian and New Zealand College of Psychiatrists
resigned as convener of its 2009 congress after his peers unanimously
voted down a proposal to dump drug company sponsorship.
The college was forced last week to appoint two co-conveners to replace
Malcolm Battersby, a fellow of the college.
http://www.theaustralian.news.com.au/story/0,25197,23463973-23289,00.html
Our skilled pharmacists are ignored. A process of epistemic capture is underway.
We are prey to vested interests. The pharmaceutical industry pervades
medical education and universities, especially postgraduate eduction,
assists with producing treatment guidelines and espouses values that
are not the same as the values demanded of the Medical Profession.
4. Doctors: remember our historic duty: Primum non nocere: Above all, do no harm.
http://www.carj.ca/issues/2006-Feb/11/11.pdf
Drug makers are public companies whose primary interest is profit. But
the new drugs for schizophrenia do work any better than old ones, some
of which have been withdrawn.From New Drugs, New Problems. Yolande
Lucire. Australian Journal of Forensic Sciences. 37:1 9-25, 2005.
The FDA trials and 52 subsequent studies evaluated in 2000, by John
Geddes of Oxford University demonstrated no clear evidence that
atypical antipsychotics were more effective or better tolerated than
conventional antipsychotics. i
Thirty-six, that being one in every 145 clinical trial subjects for
Risperdal, Zyprexa, Seroquel,) and Sertindole died; most by suicide,
yet these deaths are never mentioned in scientific literature or
prescriber information. These deaths occurred even though two thirds of
Zyprexa, nearly half the Risperdal and 80% of Seroquel subjects did not
complete the trials because the drugs were poorly tolerated. ii A rate of 27% akathisia in a trial of Zyprexa 10 mg was balanced by an equally high incidence of akathisia on placebo. iii
This indicated that Eli Lilly either did not know what they were
talking about (as akathisia is always a medication-induced phenomenon),
or the participants had not fully recovered from whatever they had been
taking before entry to the trial. Serious adverse events affected 84
subjects who took Risperdal.
None of this information
appears in promotional material. Indeed 47 serious adverse events in
87,000 users of Zyprexa injectable included eight deaths. We are being
assured that the deaths are not related to the Zyprexa but, given the
number of suicides and deaths associated with the oral preparation,
this seems to be improbable. The FDA issued a ‘black box’ warning about
sudden death from the new antipsychotic medications, (including
quetiapine and aripiprazole) but only for the elderly, in spite of
evidence that all age groups are adversely affected. vi
Further warnings are expected to advert to the extreme dangers of
mixing them with SSRIs. Nor is it the case, as suggested, that Clozaril
protects against suicide when compared with Zyprexa. Zyprexa itself is
suicidogenic. This comparison manoeuvre delays their obligation to
issue full warnings for all children and adults. The PhaRMAs are
stalling again as they did for antidepressants and as Merck did for
Vioxx, when they suggested that a high heart attack rate on Vioxx,
compared with Naproxen, occurred because the latter was protective.
David Healy has pointed out that Zyprexa and Risperdal trials had the
highest suicide rates in clinical trial history, but suicide risk does
not feature in drug company promotional material. Geodon (ziprasidone)
had the same suicide risk as SSRIs, about one in 500.
Only five Zyprexa schizophrenia trials were undertaken, but these
generated 234 ghost written articles by prominent “opinion leaders”
which were carefully placed in the prestigious journals, dependent for
their viability on PhaRMA advertising. vii
None of these publications yielded any picture at all of the risk of
suicide or suicidal acts on these drugs, let alone sudden death.
“Endorsement Science” had become the means of promotion. The colourful
capsules appeared on the cover of Time, in The Washington Times and The
New York Times. The “Dopamine Theory of Schizophrenia” was alive and
well in these endorsements, although by the time they were published it
had no more scientific validity than the serotonin theory of
depression. John Merson calls this phenomenon “epistemic capture,” the
control of knowledge by vested interests. viii
There is no protection in any mental health legislation in Australian
against doctors and Tribunals who order these drugs, which proved
intolerable to half of clinical trial subjects even for a short time,
to be enforced on community treatment order. Their side effects of
akathisia, behavioural dyscontrol, obsessive suicidality and violence
are now so common that many mental health units have been required to
employ security guards to protect themselves against their own
patients. But when so advised, and told by the patients themselves it
is my experience that many simply ignore the advice.
These figures should warn that a great number of persons are unable for metabolic reasons to take these drugs.
http://www.reuters.com/articlePrint?articleId=USL2675850920080328
And increase mortality in those treated for schizophrenia.
5. The Drugs of Concern: New Generation Antidepressants and Antipsychotics
In general terms this group of drugs are called "New Generation"
antidepressants and antipsychotics, SSRIs or SNRIs and 'Atypicals'.
The antidepressants of concern have been released serially since
1991. They are Prozac (fluoxetine) 1991, Zoloft (sertraline)
1994, Aropax (paroxetine) 1994, Luvox (fluvoxamine), Cipramil
(citalopram), Lexapro (escitalopram), Zyban (bupropion), Efexor
(venlafaxine) and Serzone (nefazodone, which was withdrawn in
2003. Some have many trade names.
The new antipsychotics, named 'atypicals', include Zyprexa (olanzapine)
and Risperdal (risperidone) and Seroquel/quetiapine, Consta/risperidone
depot.
I have too little specific knowledge to comment on Ability/aripiprazole
and Geodon/ziprasidone, other than that the same metabolic pathways are
involved.
The atypical 'antipsychotics' have been promoted for any psychosis,
which equates with 'off label' use. The Royal Australian and New
Zealand College of Psychiatrists, (RANZCP) has issued guidelines to the
treatment of schizophrenia. These guidelines conflate that disorder
with first episode psychosis – which may be a drug-induced or
medication induced state, or a schizophreniform disorder or a brief
reactive psychosis, all of whch are better left alone with minimal
symptomatic treatment. It makes little sense to treat a toxic
state with another toxin.
These guidelines suggest proactive treatment for conditions, most of which could get better more quickly if not medicated.
Some of our opinion leaders believe that early intervention can prevent
schizophrenia, which by that definition was not there before that early
intervention.
Epidemiologists can soon dismiss that claim and have done so. An
early intervention programs in Australia have only increased the
numbers of persons needing continuing health care. Some might have got
better without intervention. Some have no more then chronic side
effects.
In the USA, many doctors believe that some cases of ADHD, a socially
constructed checklist diagnosis that describes a lot of kids, are
actually cases of juvenile bipolar disorder so they apply its promoted
remedies.
Iatrogenic mental disease is common and poorly recognised. The
notion that we have collectively caused harm strikes horror in the
minds of many psychiatrists.
I refer to medication induced neurotoxic conditions, which were not
present before the vicissitudes of life were treated with drugs that
caused profound changes in brain and body.
After the Senate Inquiry into Mental Health (and others) had found a
huge increase in mental health presentations as and in suicide of
patients under mental health care, a spokesman for the Department of
Human Services in Victoria that any ‘apparent increase in suicide among
persons under mental health care has to be offset against the rising
numbers using the service.’ I have has similar reasoning put to me in
NSW as well. However the increase in persons using services and the
suicides have a common cause, which is the new drugs which have suicide
induction, akathisia and psychosis among their listed and well reported
side effects. Each completed suicide represents 10 to 20 unsuccessful
attempts, all of which increase pressure on beds.
6. Prescribing by Australian psychiatrists
'Off label' prescribing is done with the best of intentions. Off label
marketing is good for the PHaRMAs bottom line. Becausemarketed as
'antipsychotics' not as 'major tranquillisers' as were older drugs,
doctors assume that they are so called because that is what they do.
But they induce organic psychosis, (confusion, delirium) in some users,
and supersensitivity psychosis on withdrawal in some not previously
psychotic users. Many so affected are genetically
polymorphic. It is a matter of textbook psychiatry that 8% of the
population cannot be treated with antipsychotic medication and some of
them have mental illness. That is about the same number as are
poor metabolisers of drugs requiring CYP450 450 2D6. This small
population gets worse on them, hallucinates, commits suicide or
violence. If the diagnosis is of schizophrenic or bipolar is certain,
this group of 8% of 1-2% of the population is a small number. But
if toxic states (drugs) and manic shifts (from antidepressants
carelessly prescribed for stress) are misdiagnosed as serious mental
illness and this treatment is enforced on people who have already
reacted badly to a drug or substance, we soon have a public health
problem.
7. Names that hijack reasonING
Bipolar mania is rarely psychotic. However since atypicals were
licensed for it, the high incidence of psychotic side effects has
become obvious.
In drug company terms, 'frequent' means they affect more than 10% of
users. The following effects are listed in 2007 Zyprexa Product
Information (PI). (Zyprexa is licensed for bipolar disorder)
Nervous System — Frequent: abnormal dreams, amnesia, delusions,
emotional lability, euphoria, manic reaction, paresthesia, and
schizophrenic reaction;
Infrequent: akinesia, alcohol misuse, antisocial reaction, ataxia,
CNS stimulation, cogwheel rigidity, delirium, dementia,
depersonalisation, dysarthria, facial paralysis, hypesthesia,
hypokinesia, hypotonia, incoordination, libido decreased, libido
increased, obsessive compulsive symptoms, phobias, somatization,
stimulant misuse, stupor, stuttering, tardive dyskinesia, vertigo, and
withdrawal syndrome; Rare: circumoral paresthesia, coma,
encephalopathy, neuralgia, neuropathy, nystagmus, paralysis,
subarachnoid haemorrhage, and tobacco misuse.
The guidelines are silent on side effects and what doctors should do.
8. children
It is particularly pernicious that these drugs are given to children
when they have confusion, delirium and dementia among their listed side
effects. Their long-term effects have never been properly
researched. They were licensed after 6-week trials and used for
decades, without regard for long-term consequences of changes in
serotonin levels.
9. CoNsequences on public health
The public health consequences include the need for more beds for this
new population of children diagnosed with bipolar illness, which was
very rare before kids were dosed with antidepressants, antipsychotics
and various ADHD drugs, Ritalin, Adderall and amphetamines.
The resulting disturbances attracts misdiagnoses of bipolar illness and
schizophrenia, as these conditions are promoted in various ways by
those who have interests in selling remedies or increasing their power
and funding.
This is the subject of major inquiries in the United States but ignored in Australia.
http://www.naturalnews.com/018715.html
10. GENETIC VARIATIONS (POLYMORPHISMS) LEADING TO ADVERSE DRUG REACTIONS AND INTERACTIONS
http://www.fda.gov/cder/drug/drugReactions/default.htm
http://en.wikipedia.org/wiki/Eli_Lilly_Controversy
The terms pharmacogenomics and pharmacogenetics tend to be used
interchangeably. Pharmacogenetics is generally regarded as the study or
clinical testing of genetic variation that gives rise to differing
response to drugs, while pharmacogenomics is the broader application of
genomic technologies to new drug discovery and further characterization
of older drugs.
Pharmacogenetics considers genes of interest, while pharmacogenomics
considers the entire genome. (Wikipedia)
Much of current clinical interest is at the level of pharmacogenetics,
involving variation in genes involved in drug metabolism with a
particular emphasis on improving drug safety.
Responses to any medication are governed by three genetically
determined systems: transporters, receptors and cytochromes. There is
also drug sensitivity, just like allergy to penicillin, and CYP450
metabolism might be normal in those cases.
We know nothing that can as yet be clinically applied about the first
two, but genetic testing is available for CYP450 polymorphism.
Charts are available to predict reactions to and interactions between
drugs that are metabolised by CYP450. These charts go a long way to
elucidate adverse drug events, which are clinically visible but
universally unacknowledged and unrecognised in Australia.
Note that the use of one drug, such as Aropax (and other "SSRIs") can
turn a rapid metaboliser into a poor metaboliser by inhibiting
cytochrome P2D6 needed both to metabolise itself and often more so for
the second drug. That is one of the reasons that polypharmacy is
a pernicious practice. There is even a nursery rhyme that could
be about it.
There was an old lady who swallowed a cow.
I don't know how she swallowed a cow!
She swallowed the cow to catch the goat...
She swallowed the goat to catch the dog...
She swallowed the dog to catch the cat...
She swallowed the cat to catch the bird ...
She swallowed the bird to catch the spider
That wriggled and jiggled and wiggled inside her.
She swallowed the spider to catch the fly.
But I don't know why she swallowed that fly
Perhaps she'll die.
There was an old lady who swallowed a horse -
She's dead, of course.
http://kids.niehs.nih.gov/lyrics/oldlady.htm
11. WHAT DOES AN ADVERSE DRUG REACTION LOOK LIKE?
If you give drugs that target the brain, you must expect psychiatric side effects: not always those you want.
Neuroleptic toxicity (neuroleptic – called the 'neuroleptics' or drugs
that act on neurones i.e. the brain) has many faces: restlessness,
feeling terrible, wanting to tear oneself apart, blind panic, a feeling
of impending doom, insomnia, bizarre (sexual and violent) dreams,
impaired psychomotor activity, schizophrenia-like symptoms,
hallucinations, even confused beliefs and mood changes, evidence of
delirium, toxic confusion, sleepwalking, and bizarre changes in
behaviour and personality.
These reactions all occur in some patients undergoing treatment
with some psychotropic drugs. The patient gets worse, and more confused
when another psychiatric drug is added. Neuroleptic toxicity is
too frequently mistaken for the mental illness its myriad
manifestations suggest or mimic.
12. Citing my own publication, New Drugs New Problems
Other
than in rare neurological disorders or in the aftermath of epidemics of
encephalitis lethargica, akathisia is drug induced, and always
iatrogenic (caused by or resulting from medical treatment). xi
Acute akathisia may emerge after only two or three doses of an SSRI. It
is called tardive akathisia when it develops late in treatment.
Withdrawal akathisia is clinically identical and may develop up to
three months after stopping the medication.
It may be associated with a manic shift as well as rebound depression.
It does not get better unless akathisia-inducing medications are
ceased, and even then, it might take time to recede, and sometimes it
becomes chronic.
All phases cause serious distress, may compromise the psychiatric
status of the patient, may lead to impulsive actions including
aggression or self-harm, and may become chronic and resistant to
treatment. Reports ascribe to it cases of homicide and suicide.
Robert Whitaker wrote about “the madman of our nightmares” who is not a
schizophrenic but an akathisiac, having just taken, or taken himself
off, prescribed medication. Akathisia is a manifestation of brain
toxicity or altered structure. Once akathisia has set in the patient
cannot recover from whatever was there before that adverse reaction
took over.
At its extreme, akathisia can be the most painful mental state known to
humans. It was induced to torture Soviet dissidents before the 1970s
and is still used on Falung Gong in China.
(Cite source for above facts)
13. A well known Self-disclosed person: Rebekah beddoE
DEALING WITH DEPRESSION: BITTER PILLS – THEY'RE PRESCRIBED TO MILLIONS,
BUT DO THE NEW ANTIDEPRESSANTS WORK? AND ARE THEY WORTH THE RISK? BY
DANIEL WILLIAMS. TIME MAGAZINE Nov. 14, 2005.
I take this opportunity to thank Rebekah Beddoe for her generosity and her continuing assistance to sufferers. Her book, Dying For a Cure Random House 2006 should be compulsory reading for all doctors and patients.
Rebekah Beddoe didn't like the idea of
going on drugs and decided not to take them. She checked in to the
mother-and-baby unit of a private hospital, where staff helped her to
settle Jemima. There, after another brief consultation, a psychiatrist
diagnosed Beddoe with postnatal depression and suggested she start on
Zoloft right away.
This time, she relented.
A week later, she was in hospital, waiting in good spirits for a group-therapy session, when something happened.
She suddenly couldn't breathe and her heart was pounding. The walls
seemed to be closing in. She thought she was having a heart attack, but
a nurse took one look at her, disappeared for a few moments, then
returned with a paper bag that she placed over Beddoe's mouth. When
Beddoe calmed down, the nurse told her she'd had a panic attack but not
to worry - they were common in people with depression.
Beddoe's plunge into madness had begun. When a neighbour revved his
motorcycle within earshot of a sleeping Jemima, Beddoe flew into a
rage, chasing him and screaming profanities.
That night, preparing dinner, she used a knife to make shallow cuts in her left forearm, just to see how it felt.
14. Akathisia again
Since 1994, serotonin drug induced akathisia has been in the
psychiatrists' bible, the Diagnostic and Statistical Manual (DSM) of
the American Psychiatric Association. The current edition DSM IV TR:
333.99 contains the following information:
The subjective distress resulting from
akathisia is significant and can lead to non-compliance with
neuroleptic treatment. Akathisia may be associated with dysphoria,
irritability, aggression or suicide attempts.
Worsening
of psychotic symptoms or behavioural dyscontrol may lead to an increase
in neuroleptic medication dose, which may exacerbate the problem.
Akathisia can develop very rapidly after initiating or increasing neuroleptic medication.
The development of akathisia appears to be dose dependent and to be
more frequently associated with particular neuroleptic medications.
Acute akathisia tends to persist for as long as neuroleptic medications
are continued, although the intensity may fluctuate over time. The
reported prevalence of akathisia among individuals receiving
neuroleptic medication has varied widely (20%-75%).
15. WHAT IS BEHAVIOURAL DYSCONTROL OR BEHAVIOURAL TOXICITY?
The following was all known twenty-eight years ago about all
psychiatric drugs. All has since been largely forgotten. Why does
a whole generation of psychiatrists not know about it? From
Comprehensive Textbook of Psychiatry III (1980, eds. Kaplan, Freedman
& Sadock), p. 2284:
The term “behavioural toxicity” has been applied to adverse behavioural change produced by a psychotropic drug.
It is often difficult to evaluate such a change in seriously ill
schizophrenic patients, since it would be necessary to clearly separate
non drug-related worsening of the schizophrenic state from drug-induced
toxicity.
Symptoms such as insomnia, bizarre dreams, impaired psychomotor
activity, aggravation of schizophrenic symptoms, toxic confusional
states and somnambulism do occur in patients undergoing treatment with
psychotropic drugs.
In addition, patients differ in their rate of metabolism of a specific
drug, and slow metabolizers may build up psychotoxic levels of drugs or
metabolites.
In 1980 it was textbook psychiatry that individuals metabolised drugs differently.
Most of the drugs used in psychiatry, and some other medicines (and
this is very general) are metabolised in the liver by an enzyme system
called cytochrome P450.
The undergraduate, short version of DSM III(1980) aplan and Sadock contained this information:
Akathisia is a subjective desire to be in
constant motion. A manifestation of drug sensitivity, it may be
confused with psychotic agitation and incorrectly treated by increasing
the dose of the offending medication.
The symptom subsides promptly when the offending medication is
discontinued and replaced by another one better tolerated by the
patient.
16. REBEKAH BEDDOE
If acute akathisia is unrecognised it becomes chronic, and recurs again
and again in the course of treatment. Beddoe's story continues, in Time
Magazine.
Over time, her psychiatrist added tranquilizers, an extra antidepressant, lithium and eventually an antipsychotic to Beddoe's diet of drugs. There was also a course of electroconvulsive therapy.
But her condition worsened. In 2000 she tried to end her life by
overdosing on sleeping pills, the first of four such attempts.
At her mother's urging she switched psychiatrists, but after stripping back her regimen to a single drug, Prozac,
the new doctor gradually built it up again. Beddoe developed akathisia,
which she describes "as a horrible energy that fills you with angst and
dread and propels you to move about constantly." Akathisia can be
a manifestation of SSRI sensitivity, and "it's psychiatry's dirty
little secret, "says skeptic Lucire."
But Beddoe's
psychiatrist saw it as just another symptom of his patient's illness.
Beddoe's behaviour is a typical acute akathisia response such as occurs
not only in response to Zoloft but to any antidepressant or
antipsychotic to which the user is sensitive. Its elements are intense
dysphoria (meaning the patient feels awful) panic, violence in thought
and deed directed at self or others, substance-induced delirium (in
this case induced by medication), complicating or mimicking a mental
illness, and behavioural toxicity.
17. Akathisia in wikipedia
The definition of akathisia in wikipedia is among the best for the polymorphic condition with many faces.
Akathisia (or "acathisia") is an often
extremely unpleasant subjective sensation of "inner" restlessness that
manifests itself with an inability to sit still or remain motionless,
hence the origin of its name: Greek a (without) + kathisis (sitting).
It is a common side effect of certain drugs, notably typical or
atypical antipsychotics (also called major tranquillisers), such as
haloperidol (Haldol®) and droperidol, olanzapine (Zyprexa®); SSRIs,
such as paroxetine (Paxil®); tricyclic antidepressants, certain
antihistamines, such as promethazine and diphenhydramine (Benadryl®);
and certain anti-emetic drugs, particularly the dopamine blockers (e.g.
metoclopramide (Reglan®) and prochlorperazine (Compazine®)).
Akathisia may range in intensity from a mild sense of
disquiet or anxiety (which may be easily overlooked) to a total
inability to sit still, with overwhelming anxiety and severe dysphoria
(manifesting as an almost indescribable sense of terror and doom). In
the most severe cases, dysphoria can be so severe that the patient is
literally compelled to take action, leading, possibly, to suicide
attempts. It is not unknown to have patients literally run out of a
hospital or emergency room.
Akathisia is often misdiagnosed and can lead the patient to commit suicide in or outside the hospital.
Causes:
*typical or atypical antipsychotics (also called major tranquillisers),
such as haloperidol (Haldol®) and droperidol, olanzapine (Zyprexa®);
*SSRIs, such as paroxetine (Paxil®);
*Tricyclic antidepressants, certain antihistamines, such as
promethazine and diphenhydramine (Benadryl®); and certain anti-emetic
drugs, particularly the dopamine blockers (e.g. metoclopramide
(Reglan®)(Maxolon) and prochlorperazine (Compazine®)).
Treatment includes discontinuation or reduction of dose of the
causative agent, and the use of typical or atypical antipsychotics
(also called major tranquillisers) to reduce the agitation and anxiety.
Unfortunately, these neuroleptics are often the cause of the condition
and are known to cause irreversible akathisia in some cases. While the
administration of these drugs may temporarily ameliorate the symptoms,
there is a serious risk of worsening the condition over the long term.
Most of the clinical cases of akathisia can be prevented by not administering the drugs that cause the condition.
18. ADVERSE DRUG REACTIONS FROM GENELEX SEE BELOW FOR LINK.
Adverse drug reactions (ADRs), usually called side effects, are a long-standing and largely neglected major medical problem.
These are not medical errors. They occur within the US Food and Drug
Administration (FDA) approved dosage and labelling recommendations. The
recently reported problems with antidepressant-induced teen suicides,
the recalls of Vioxx and Baycol and the upgrading of Accutane
monitoring by the FDA are the tip of the iceberg.
19. INCIDENCE OF ADVERSE DRUG REACTIONS
This comes for the www.genelex.com website
ADRs are the fourth to sixth greatest killer
in the US, with more than 100,000 deaths per year; and 2.2 million
serious adverse reactions per year according to a 1998 Journal of the
American Medical Association report (JAMA 279:1200 1998). This study is
a meta-analysis of 39 research reports published from 1966 to 1996.
21.3% of the 548 most recently FDA approved medications were
subsequently withdrawn from the market or given a black box warning.
(JAMA 287:2215 2002)
The Government Accountability Office reports that 51% of new drugs have
serious, undetected adverse effects at the time of approval.
Of the best selling prescription drugs, 148 can cause
depression, 133 hallucinations or psychoses, 105 constipation, 76
dementia, 27 insomnia and 36 parkinsonism. (Worst Pills Best Pills: A Consumers Guide to Avoiding Drug-Induced Death or Illness, 3rd ed., 1999)
20. FINANCIAL CONSEQUENCES
$1.77 billion in added health care costs per year (Journal of the American Pharmaceutical Association 41:192 2001)
Health maintenance organisations spend more treating ADRs than on drugs.
Attention: Medical Benefits Funds in Australia. You can stop insurance money being wasted.
Adverse Drug Reactions are the cost leader for malpractice payouts.
Up to one third of drug prescriptions are not needed and therefore wasted.
http://www.fda.gov/c
der/aers/default.htm
Has anyone talked to Medical Benefits funds?
Has anyone noticed Workcover statistics? Psychological injury is
increasing annually. And suicides in WorkCover claimants. Why? They
were fully functional workers with industrial problems before they were
medicalised.
NSW WorkCover Mental disorder cases by gender, 1992/3 to 2004/5
Year |
Males |
Females |
Total |
% of all diseases |
% of all claims |
Incidence rate |
1991/92 |
299 |
174 |
473 |
4.8 |
0.9 |
0.2 |
1992/93 |
366 |
278 |
644 |
5.4 |
1.3 |
0.3 |
1993/94 |
597 |
512 |
1,109 |
6.9 |
1.9 |
0.5 |
1994/95 |
784 |
804 |
1,588 |
9.4 |
2.5 |
0.7 |
1995/96 |
752 |
986 |
1,738 |
10.7 |
2.8 |
0.8 |
1996/97 |
720 |
867 |
1,587 |
13.9 |
2.6 |
0.7 |
1997/98 |
875 |
1,033 |
1,908 |
18.8 |
3.3 |
0.8 |
1998/99 |
736 |
946 |
1,682 |
17.6 |
3.0 |
0.7 |
1999/00 |
711 |
866 |
1,577 |
17.2 |
3.0 |
0.6 |
2000/01 |
829 |
1,087 |
1,916 |
20.7 |
3.6 |
0.7 |
2001/02 |
1,151 |
1,492 |
2,643 |
26.8 |
4.8 |
1.0 |
2002/03 |
1,396 |
1,850 |
3,246 |
35.4 |
6.4 |
1.2 |
2003/04 |
1,330 |
1,896 |
3,226 |
33.6 |
6.3 |
1.2 |
2004/05 |
1,259 |
1,943 |
3,202 |
? |
6.4 3 |
1.24 |
|
Note females have overtaken males as they nearly have in suicide
data. Different metabolism in females, slower perhaps, as with
Zyprexa?
My own series indicates that most got antidepressants and side effects and stayed sick, sometimes catastrophically so.
http://www.healthanddna.com/drugchart.html
There are genetic, biological differences between individuals, some of
whom do not produce certain cytochromes at all. Many patients do not
respond to drugs and/or experience adverse drug reactions. 25% of the
most commonly prescribed drugs, antidepressants, antipsychotics and
antiepileptics, are metabolised by CYP2D6 and 2C19, and 2C9.
In practice this means that somewhere between 7% and 14% of Caucasians
who are born with no 2D6, or very little of it, cannot metabolise
certain drugs, for example, SSRIs, at all or they do it slowly. 2D6 is
one of several cytochromes that are different in different people. They
have responses like Beddoe's.
21. SO HOW COMMON ARE ADVERSE EFFECTS FROM NEW ANTIDEPRESSANTS?
http://www.psychotropical.com/1_cyp_introduction.shtml
http://www.healthanddna.com/drugchart.html
http://www.lucire.com.au/documents/Cytochromes-paradigmatic.aspx
Again, from TIME MAGAZINE
Even doctors who swear by SSRIs and
newer variants concede that 1–2% of patients have a severe negative
reaction to these drugs. That's a small percentage. But it's a small
percentage of a very large number. Intractable misery is rife, it
seems: in Australia last year, 12 million prescriptions for
antidepressants were dispensed through the federal government's
Pharmaceutical Benefits Scheme (up from 8.2 million in 1998), a figure
equating to more than a million users. Do the math, says Sydney
forensic psychiatrist Yolande Lucire: if only 1% of users suffer
terrible side effects that aren't recognized for what they are, that's
more than 10,000 Australians who've recently been disabled by a drug
that was supposed to help them. "That would be enough to fill the beds
in every mental hospital in the country."
1–2% is a very conservative estimate. Clinical trials have shown
that it is more like 27% and one in ten, at a minimum, becomes suicidal.
One in 500 died of suicide in those clinical trials that had been
published before 2003, as analysed by David Healy in this paper.
There has been a long-standing
controversy about the possibility that selective serotonin reuptake
inhibitor (SSRI) antidepressants might induce suicidality in some
patients. To shed light on this issue, this paper reviews available
randomized controlled trials (RCTs); meta-analyses of clinical trials
and epidemiological studies that have been undertaken to investigate
the issue further. The original clinical studies raising concerns about
SSRIs and suicide induction produced evidence of a dose-dependent link
on a challenge-de-challenge and rechallenge basis between SSRIs and
both agitation and suicidality. Meta-analyses of RCTs conducted around
this time indicated that SSRIs might reduce suicidal ideation in some
patients. These same RCTs, however, revealed an excess of suicidal acts
on active treatments compared with placebo, with an odds ratio of 2.4
(95% confidence interval 1.6–3.7).
This excess of
suicidal acts also appears in epidemiological studies. The data
reviewed here make it difficult to sustain a null hypothesis that SSRIs
do not cause problems in some individuals. Further studies or further
access to data are indicated to establish the magnitude of any risk and
the characteristics of patients who may be most at risk.
http://www.lucire.com.au/documents/pdf/HealyWhitaker.pdf
We now know that the trials where the drug did not do well were never revealed.
At a minimum, the rate that such adverse reactions will occur is
consistent with the number of poor metabolisers, 7–14% of 2D6.
When one adds in poor metabolisers for other CYP450 isoenzymes, it can
be 50%. Antidepressants inhibit 2D6 and make it difficult for any but
ultrarapid metabolisers to take more than a single dose and to tolerate
more then one drug that demand 2D6 for its metabolism.
About 8% of Caucasians cannot metabolise these drugs at all. They
simply lack one essential enzyme, 2D6, some completely and some are
very short of it and it cannot be induced. About half the
population has difficulties taking a high dose or being on more than
one drug. Cannabis renders normal metabolisers effectively polymorphic
by inducing 1A2.
Those who cannot metabolise antidepressants and antipsychotics develop
serious adverse side effects – including sudden death. Some commit
suicide or homicide after only a few doses as their blood levels
rapidly become elevated and the brain and body become toxic.
Most people stop taking the drug immediately they feel awful on it, as
did clinical trail subjects, but in hospital they are not permitted to
do so and on treatment orders they are forbidden to do so. They may
develop vomiting and diarrhoea, as 95% of the serotonin is in the body,
and only a small amount in the brain. Sometimes the body's rejection of
the drug is treated with Stemetil of Maxolon, (both akathisia inducers)
with disastrous results. Most fail to recognise effects in themselves
because of their organically impaired condition.
Breggin has previously proposed the brain-disabling principle of
psychiatric treatment that all somatic psychiatric treatments impair
the function of the brain and mind. Intoxication anosognosia
(medication spellbinding) is an expression of this drug-induced mental
disability.
Intoxication anosognosia causes the victim to
underestimate the degree of drug-induced mental impairment, to deny the
harmful role that the drug plays in the person's altered state, and in
many cases compel the individual to mistakenly believe that he or she
is functioning better.
In the extreme, the individual displays out of character compulsively
destructive behaviours, including violence toward self and others.
http://www.breggin.com/spellbinding_psychiatric_drugs_abstract.html
http://psychrights.org/articles/articles.htm
http://en.epochtimes.com/news/7-4-20/54369.html
Drug interactions are not the subject of black box warnings in
Australia, and there is no system for teaching doctors in the community
about them.
http://www.mja.com.au/public/issues/179_11_011203/man10667_fm.html
Adverse drug reactions and interactions are rarely a subject of
continuing medical education, most of which is conducted at
drug-company funded conferences and seminars.
http://www.pharmalot.com
Subject: Drug promotion disguised as "independent" medical seminars:
www.theaustralian.news.com.au/story/0,25197,23255729-2702,00.html
Also an interview for Radio National. A transcript is available at:
http://www.abc.net.au/am/content/2008/s2169583.htm
Drug interactions can be found by consulting prescribing manuals and
combining the known effects. But there is a shortcut: Google on the
Internet will disclose most of them, in a fraction of a second. Some
understanding is needed of metabolic pathways, which deal with these
drugs in the body.
22. THE BACKGROUND: WHAT IS HAPPENING IN MENTAL HEALTH IN NSW, IN AUSTRALIA IN THE EARLY TWENTY-FIRST CENTURY?
MORE PATIENTS, MORE SUICIDES, MORE VIOLENCE AND MORE BEDS
In June of 2003, Professor Beverley Raphael, Director of the NSW
Centre for Mental Health, told The Bulletin that the numbers of people
requiring psychiatric treatment fronting at hospital emergency
departments had doubled in the past decade.
Nobody asked why, or whether this was real or apparent, or what this
new seriously mentally ill population was really suffering from. The
incidence of schizophrenia, biological depression and bipolar disorder
(diagnosed according to international criteria) has been constant over
the last century and across cultures. Yet NSW appeared to have twice as
many persons with mental illness serious enough to present at emergency
departments than were presenting before 1992.
The new population demanding mental health services was also more
suicidal and more violent. The Bulletin went on to describe changes:
About 400 mentally ill patients
throughout Australia – most of them aged in their 20s and 30s – will
commit suicide this year because the places that once treated them have
been closed or diminished. They are being turned away and sent to their
deaths.
Increasing resources and bed numbers has done little for the problem, as exemplified by a rural unit, described later.
The Bulletin article written by Hall Greenland, in August 2003, continued:
When a cluster of nine homicides by
recently discharged psychiatric patients occurred in NSW in 2001, the
NSW Centre for Mental Health sent for (Dr. Bill Barclay, a very senior
forensic psychiatrist.... Violent and suicidal, Hossam Attia tried to
kill himself by driving his car into a wall. After being admitted to
hospital, he was assessed by two psychiatrists as being at high risk of
doing harm to himself and his family, and was recommended for hospital
treatment. Two days later, another two psychiatrists (without
consultation with Hossam’s wife or their colleagues) gave him a
prescription for anti-depressants and let him loose. He went home and
shot his wife, then himself. Their three children were in the house at
the time. Asked later by the coroner why they discharged him, the
doctors replied: “Risks of suicide and harm to others were considered
high. However, community management was considered the least
restrictive option.”
By 2003, the connection between antidepressants and suicide/homicide
was well established internationally, and few of us have not seen this
problem in our patients, colleagues, friends and neighbours. The
Wesbecker/Forsyth case (see below) had been written up in the national
newspaper The Australian in 1996. Such reports appear daily in the
international press. But the fact that the perpetrators of massacres
were on psychiatric drugs, which drugs they were on or were in
withdrawal from, is not reported in Australian newspapers.|
The Bulletin report can be accessed at
http://livesworthyoflife.com/uploads/File/Greenland-Dyingshame.pdf
The case of the 72-year-old Mr Hawkins, who killed his wife after
having Zoloft prescribed (for little more than feeling out of sorts),
was decided in the NSW Supreme Court in 2000.
http://caselaw.lawlink.nsw.gov.au/isysquery/irl2742/1/doc
Dr Healy’s views as to the effects
of Zoloft have particular weight since his doctoral thesis was based on
research on the serotonin transporter system and the role of serotonin
in depression and suicide. In this regard it should be noted that
Zoloft is a serotonin re-uptake inhibiter. His interest in serotonin
re-uptake inhibitors has been ongoing. Furthermore, he has carried out
research and clinical work on existing and novel psycho-pharmacological
drugs and is an author in the field of psychopharmacology. His opinion
is also supported by an assessment of suicidal acts of patients on
sertraline prepared in response to an inquiry from the Irish Medicines’
Board in 1999, and by a study in healthy volunteers conducted in the
College of Medicine in the University of Wales using a dose of only 50
mgs of Zoloft. Two subjects with no prior history of mental or
psychiatric problems and no current problems became suicidal and
aggressive on such a dose of Zoloft. This was said by Dr Healy to be:
“Significant in that it demonstrates that such problems can occur in an entirely normal individual.”
Psychiatrists were in denial, or not reading the newspapers.
Over 2,000 more such tragic cases of homicides, family homicides,
senseless and often multiple homicides, suicides, weird crimes and
serious adverse drug events and some of their legal defences are
documented from media reports around the world at www.ssristories.com And more at http://ssri-uksupport.com/files/homicidesSSRISandADHDmedications.pdf
D, Herxheimer A, Menkes DB (2006). "Antidepressants and violence:
problems at the interface of medicine and law". PLoS Med. 3 (9): e372.
Several cases have been extensively analysed.
http://medicine.plosjournals.org/perlserv/?request=get-document&doi=10.1371%2Fjournal.pmed.0030372
Also link to Let Them Eat Prozac – The Trials
The original group of litigated mass 'SSRI' homicides and suicides
complete with Daubert Hearings, court transcripts and experts'
depositions (evidence) can be seen on the website of Professor David
Healy with the following link: http://www.healyprozac.com/Trials/default.htm
23. AN INTERNATIONAL EPIDEMIC OF PSYCHIATRIC DISABILITY
The problem is not only Australian. Robert Whitaker writes:
Over the past 50 years, there has been an astonishing increase in severe mental illness in the United States.
The
percentage of Americans disabled by mental illness has increased
fivefold since 1955, when Thorazine, remembered today as psychiatry's
first "wonder" drug was introduced into the market.
The
number of Americans disabled by mental illness has nearly doubled since
1987, when Prozac – the first in a second generation of wonder drugs
for mental illness – was introduced. There are now nearly 6 million
Americans disabled by mental illness, and this number increases by more
than 400 people each day.
A review of the scientific
literature reveals that it is our drug-based paradigm of care that is
fuelling this epidemic. The drugs increase the likelihood that a person
will become chronically ill, and induce new and more severe psychiatric
symptoms in a significant percentage of patients.
http://www.psychrights.org/Articles/EHPPPsychDrugEpidemic(Whitaker).PDF
24. THE AUSTRALIAN EXPERIENCE: CHEAP MEDICINES AND FREE HEALTHCARE AND NO CONTROLS ON PRESCRIBING
From my own practice, I have reported on homicides, attempted
homicides, scores of suicide attempts, completed suicides and assaults,
as well as peculiar crimes, various manias, dipsomania, kleptomania,
erotomania, gambling mania, as well as sexual crimes by improbable
offenders, in a serried of cases involving over 500 hospital admissions
for akathisia, suicidality, homicidal thinking and violence, in over
400 individuals, some of whom were admitted thirty or more times. Cases
treated in private practice or reported to courts are rarely reported
in the press.
Medical confidentiality is a fine thing in itself, but it may be an
impediment to progress if one is not permitted to write up information
generated in the public sector. No personal details are required to do
this, only medications and responses.
Australia seems to be behind the UK and USA in recognising and
dealing with this public health problem. It seems to be a problem in
the United States as well, where disability from psychiatric causes has
increased. Three years ago, the identification and retrieval of these
patients was occupying the Royal College of Psychiatrists.
Also going up and up from 1992 were numbers and rates of hospitalised
suicide attempts, as documented in the Annual Report of the New South
Wales Chief Health Officer. These increased from 55 per 100,000 to 155
per 100,000. This information can be accessed by the link: http://www.health.nsw.gov.au/public-health/chorep/men/men_suihos.htm
In that report note the numbers of young females. Females, particularly
young ones, metabolise Zyprexa/olanzapine and perhaps other medicines
poorly. Females now figure too prominently in suicide numbers, where
they were formerly outnumbered four to one by men. Suicides on
antidepressants involve equal numbers of men and women, whereas in
national statistics, men outnumber women in a ratio of 4:1.
It is interesting to note that there are recorded instances where the
introduction of psychiatric services to a developing country that
previously did not have such services, in fact increases its suicide
rate. The study concludes that it is of concern that most mental health
initiatives are associated with an increase in suicide rates.
http://www.blackwell-synergy.com/doi/abs/10.1111/j.1440-1614.2004.01484.x
The authors try to find an explanation for this phenomenon, one that
avoids blaming psychiatry and its remedies. Following is a statement
from a textbook of psychiatry published over 40 years ago. It refers to
observations in patients during initial treatment with tricyclic
antidepressants [Clinical Psychiatry, by Mayer-Gross, Slater, and Roth,
1960, p. 231]:
With beginning convalescence (following
initiation of treatment with tricyclic antidepressants), the risk of
suicide once more becomes serious as retardation fades.
This British textbook, my undergraduate book, was cited in the recent FDA review of antidepressant suicidality.
http://www.fda.gov/OHRMS/DOCKETS/AC/06/briefing/2006-4272b1-01-FDA.pdf
We would now call this condition and its energised or 'manic
suicidal' state 'acute akathisia', but we knew nothing about akathisia
in the 1950s, only that some patient treated for depression killed
themselves very suddenly and without warning, the drugs in use were tri
and tetracyclics. (TCAs)
The inherent risk that a patient will experience this phenomenon
provides a reason to limit any anti-depressant treatment to a small,
well focused, high risk group of biologically depressed persons and to
increase the dose slowly, to watch and warn and supervise carefully. As
suicide epidemiologist Ronald Maris has shown, new antidepressants are
up to six times more likely to cause suicide than old ones, which are
not innocent either.
http://www.fda.gov/cder/drug/antidepressants/antidepressants_MG_2007.pdf
Akathisia is but one of several mechanisms that have been proposed to
explain the clinical observation that some patients being treated with
antidepressants, particularly early in treatment, may have an increase
in suicidality. This FDA study of 372 clinical trials, which looked at
suicides on active substance and not in withdrawal reports:
This has been a major effort, involving
372 placebo-controlled antidepressant trials and almost 100,000
patients. The purpose of the December 13th 2006 meeting is to update
the committee with our findings from this meta-analysis. We will
present our findings and our interpretations of the data, and we will
generally discuss our plans for labelling modifications based on these
findings
This review does not look at suicides in the withdrawal phase, so
one can halve the numbers on 'placebo’; and double the suicide numbers
responding to or on antidepressants. Nonetheless the figures associated
with venlafaxine and paroxetine, even without relocating some placebo
suicides as medication-withdrawal phase suicides, carry serious
implications but are consistent with the peer-reviewed literature.
But in 2008, we have yet to hear something from the Australian
equivalent of the US FDA, the Therapeutic Goods Administration (TGA) or
get updated advisories or letters from drug companies to tell us of the
massive paradigm shift. Australians are being taken for suckers.
Dr Jean Lennane told The Bulletin that 20-30 was the number of annual
suicides under mental health care before 1992. This number has
increased hugely since that time, peaking in 1997 after the
introduction of several new medicines. Psychiatric services are the
equivalent of giving drugs.
http://amwac.health.nsw.gov.au/pubs/2005/track_trag_06.html
Extract: Reported suicide deaths of patients in contact with mental health services, and all suicide deaths in NSW 1993-2001
http://www.blackwell-synergy.com/doi/abs/10.1111/j.1440-1614.2004.01484.x
http://amwac.health.nsw.gov.au/pubs/2005/track_trag_06.html
Extract: Reported suicide deaths of patients in contact with mental health services, and all suicide deaths in NSW 1993-2001
Year |
Suicides in NSW |
Suicides in mental
Health care |
Percentage of all
Suicides |
1992 |
|
|
9% |
1993 |
676 |
68 |
10% |
1994 |
798 |
72 |
9% |
1995 |
747 |
100 |
13% |
1996 |
811 |
136 |
17% |
1997 |
946 |
166 |
18% |
1998 |
827 |
143 |
17% |
1999 |
846 |
173 |
20% |
2000 |
738 |
156 |
21% |
2001 |
775 |
159 and 156 in 2002 |
21% |
|
25. CHILDREN
NSW has built approximately 500 new mental health beds since 1992. The
increasing demand for mental health beds is described by an audit
accessed at
http://www.google.com.au/search?hl=en&q=mental+health+beds+NSW&btnG=Google+Search&meta
http://www.audit.nsw.gov.au/publications/reports/performance/2005/mental_health/inbrief.pdf
NSW has a further 1100 beds on the drawing boards, some of which are for adolescents.
Adolescents are badly affected by antidepressants and antipsychotics
– this is subject of many Advisories and Black Box Warnings. Only
Prozac is licensed for children, but 'off label' prescribing of all
antidepressants and of antipsychotics not licensed for kids is rife in
Australia, to the extent that new mental health units for adolescents
have had to be built.
http://www.fda.gov/cder/drug/antidepressants/historical.htm
Further information about the rising numbers of suicides and homicides
by people under mental health care can be accessed by examining
Tracking Tragedy: the annuals Reports of the Sentinel Events Committee
2003, 2004, 2005. The Sentinel Events Committee looked at all factors
other than recent and current medication. The link is:
http://parliament.nsw.gov.au/prod/la/latabdoc.nsf/0/9F8D48CCE0DBB525CA25737E003C1E60
Or for former reports
http://www.google.com.au/search?hl=en&q=Tracking+tragedy&btnG=Google+Search&meta
The relative risk of suicide against placebo by these drugs was
reported by Maris in 2002, and can be accessed by the link below. This
much was known in 2002.
http://psychrights.org/Research/Legal/Evidence/MarisonSSRIsUnderDaubert.htm
This information has been published in peer-reviewed journals by David Healy.
Table 1: Incidence of Suicides and Suicide Attempts in Antidepressant Trials Submitted to FDA
| Investigational Drug |
Patient No |
Suicide No |
Suicide Attempt No |
Suicides and Attempts as a % of Patient Numbers |
| Sertraline
Active comparator
Placebo
Placebo Washout |
2,053
595
786 |
2
0
0
0 |
7
1
2
3 |
0.44%
0.17%
0.25% |
| Paroxetine
Active comparator
Placebo
Placebo Washout |
2,963
1151
554 |
5
3
0
2 |
40
12
3
2 |
1.52%
1.30%
0.54% |
| Nefazodone
Active comparator
Placebo |
3,496
958
875 |
9
0
0 |
12
6
1 |
0.60%
0.63%
0.11% |
| Mirtazapine
Active comparator
Placebo |
2,425
977
494 |
8
2
0 |
29
5
3 |
1.53%
0.72%
0.61% |
| Bupropion
Placebo |
1,942
370 |
3
0 |
----
---- |
|
| Citalopram
Placebo |
4,168
691 |
8
1 |
91
10 |
2.38%
1.59% |
| Fluoxetine
Placebo
Placebo Washout |
1,427
370 |
1
0
1 |
12
0
0 |
0.91%
0.00% |
| Venlafaxine
Placebo |
3082
739 |
7
1 |
36
2 |
1.40%
0.41% |
| All new drugs
All SSRIs
Total Placebo |
21,556
13,693
4,879 |
43
23
2 |
232
186
21 |
1.28%
1.53%
0.47% |
|
For the sources of this data:
http://www.ahrp.org/risks/healy/FDA0204.php
http://www.healyprozac.com/EditorsDilemma/Psychotherapy_Psychosomatics.pdf
And is the craze over now?
http://www.guardian.co.uk/society/2008/feb/27/mentalhealth.health1?gusrc=rss&feed=worldnews
26. WHY IS EVIDENCE FROM CLINICAL TRIALS SO IMPORTANT?
Clinical trials are important because they are designed to tell us how
a drug will perform when it is it is released into the community. If
placebos do better then the drug it will cause problems.
In practice, it will actually not do as well as it appeared to do in the trials.
Many more start the trials than finish them, so a lot of people who cannot tolerate the drug simply drop out.
We are told only of those who stayed in until the end. We are
told only of the best trials. Where the drug did not do well is simply
not disclosed.
In clinical trials, subjects see a rater each week. The rater knows
what side effects are and pulls out subjects who exhibit them. We are
not told of the dropouts, so we do not have a proper idea of how the
drug is tolerated by a random population.
In clinical trials only one drug is being taken.
In the clinical setting, patients are often taking more than one
drug, but in the clinical setting side effects are often not recognised
as such. The patient who becomes hallucinated on an antidepressant will
get an antipsychotic requiring the same metabolic pathway and making
her condition even worse.
The patient who develops diarrhoea or vomiting (serotonergic side effects) might get an antiemetic.
The patient with antidepressant-induced hypertension is treated with
an antihypertensive. Instead of withdrawal of the culprit drug, each
complicating symptom might get its own remedy, and it all gets worse.
Such polypharmacy (use of multiple medications) is almost inevitable in hospitals.
27. LITIGATION IN USA – ASK ELI LILLY TMAP
Congressional hearings in the USA have revealed the disparity between
the knowledge held by (pharmaceutical companies) and the information
they disclose in their advertising.
New York’s former Attorney General, Eliot Spitzer, now
Governor, won a settlement of $US 430 million against Warner Lambert, a
subsidiary of Pfizer Inc., for illegal and deceptive promotions of one
of its blockbuster drugs, Neurontin.
A score of US State attorneys have followed suit, expecting windfall
income for state coffers to recoup some of the healthcare costs
generated by the indiscriminate use of these drugs.
“It is critically important that
physicians and their patients receive fair, balanced and accurate
information about prescription drugs and the conditions these
medications are approved to treat,” Spitzer said. “Marketing strategies
that deceptively and illegally promote drugs for unapproved purposes in
order to increase a pharmaceutical company's bottom line will be
aggressively investigated.” xii
Spitzer conducted the first successful litigation against
GlaxoSmithKline (GSK) for non-disclosure of risk, specifically in the
case of Aropax. He obtained an undertaking by pharmaceutical companies
to place details of clinical trials, even those previously undisclosed,
on the Internet. Most have failed to comply, but Eli Lilly information
or at least summaries of it are is available on www.lillytrials.com and it took four more years before GSK disclosed the suicide rates in clinical trials for Aropax in adults.
An Area Health Service can counter-sue pharmaceutical companies.
For example, GSK failed to disclose relevant information about suicide
caused by Seroxat/Paxil/Aropax/paroxetine in persons under 30, while
denying that this happened in older persons. There were six suicides in
the clinical trails conducted by GSK in young persons being treated
with Aropax for social anxiety disorder (psychobabble for shyness), see
below and none among those on placebo.
This is more than a six-fold increase: 6 suicides to none is infinitely
more than sixfold. Shy people do not commit suicide. See below a
link to a ‘Dear Doctor’ letter from GSK. I for one am still waiting to
receive such a letter from an Australian regulator.
http://www.fda.gov/MedWatch/SAFETY/2004/Paxil_hcp.pdf
And what GSK did not disclose is now available:
http://www.gsk.com/media/paroxetine/adult_hcp_letter.pdf
In February 2008 it was uncovered that, again, GSK criminally and
catastrophically failed to reveal an eightfold increase in suicide in
clinical trials for adults.
An analysis of internal GSK memos and
reports, which were released to US lawyers seeking damages, suggests
that the company had trial data, demonstrating an eightfold increase in
suicide risk as early as 1989. Harvard University psychiatrist Joseph
Glenmullen, who studied the papers for the lawyers, says it's
"virtually impossible" that GSK simply misunderstood the data – a claim
the company describes as "absolutely false."
http://www.newscientist.com/channel/health/mg19726424.600-did-gsk-trial-data-mask-paxil-suicide-risk.html
See Dr. Glenmullen's report at:
http://media.newscientist.com/data/images/ns/av/mg19726424600D1.pdf
http://www.bmj.com/cgi/content/full/333/7558/92
These postings on the FDA website have forensic utility to show the
extent to which the advertising differs from what was found in clinical
trials presented for licensing purposesxiii.
However the FDA is not well regarded in the USA. It is beholden to
clients, the pharmaceutical industry and riddled with conflicts of
interest. The TGA was similar placed into a client relationship with
drug companies and Mr Tony Abbott, the federal Health minister,
announced that at a post budget presentation in 2005 at a function at
the Sydney Opera House funded by Pfizer.
An excellent overview of FDA's failure to function as a public interest
watchdog -as is its legal mission- appears in the current issue of The
Readers Digest (below).
"Lurching from one disaster to
another, the 102-year-old agency learns of dangers too late and then
moves too slowly to remedy them. Instead of depending on the FDA,
Americans are doubting it -- and for good reason."
The
greatest concern is drug safety. FDA's financial dependence on
pharmaceutical company user fees has led FDA leadership to regard
industry-rather than the public--as the agency's "clients." The
consequences of this mindset can be measured in hundreds of thousands
of preventable tragedies, including deaths. From veracare@ahrp.org, ALLIANCE FOR HUMAN RESEARCH PROTECTION Promoting Openness, Full Disclosure, and Accountability
Reader's Digest
Strong Medicine: What's Ailing the FDA
http://www.ahrp.org and http://ahrp.blogspot.com
http://www.rd.com/national-interest/special-reports-and-surveys/problems-in-the-fda/article.html
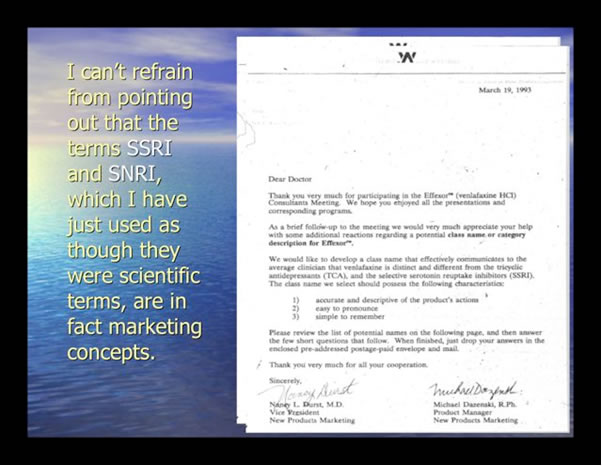
28. WHERE DOES FRAUD START?
Professor Edward Shorter, a historian of medicine, often shows the
following documents in slides, demonstrating that the names of these
drugs were no more than marketing ploys, and did not reflect their
actions.
I
can’t refrain from pointing out that the terms SSRI and SNRI, which I
have just used as though they were scientific terms, are in fact
marketing concepts.
|
Dear Doctor,
March 19, 1993
Thank
you very much for participating in the EffexorTM (venlafaxine HCI)
Consultants Meeting. We hope you enjoyed all the presentations and
corresponding programs.
As a brief follow-up to the
meeting we would very much appreciate your help with some additional
reactions regarding a potential class name or category description for
Effexor.
We would like to develop a class name that
effectively communicates to the average clinician that venlafaxine is
distinct and different from the tricyclic antidepressants (TCA), and
the selective serotonin reuptake inhibitors (SSRI). The class name we
select should possess the following characteristics:
accurate and descriptive of the product’s actions
easy to pronounce
simple to remember
Please
review the list of potential names on the following page, and then
answer the few short questions that follow. When finished, just drop
your answers in the enclosed pre-addressed postage-paid envelope and
mail.
Thank you very much for all your cooperation.
Sincerely,
Nancy L Durst, MD
Vice President
New Products Marketing |
Michael Dazenski, R.Ph
Product Manager
New Products Marketing |
|
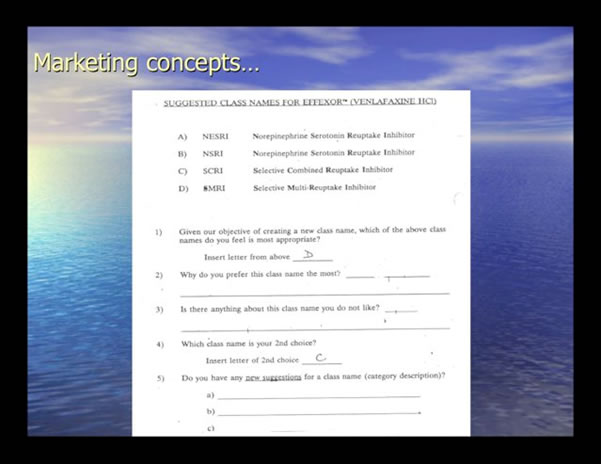
Marketing Concepts
SUGGESTED CLASS NAMES FOR EFFEXOR™ (VENLAFAXINE HCI)
A) NESRI Norepinephrine Serotonin Reuptake Inhibitor
B) NSRI Norepinephrine Serotonin Reuptake Inhibitor
C) SCRI Selective Combined Reuptake Inhibitor
D) SMRI Selective Multi Reuptake Inhibitor
1) Given our objective of creating a new class name which of the alternate class names do you feel is most appropriate?
Insert letter from above _______
2) Why you prefer this class name the most?
3) Is there anything about the class name that you do not like
4) What class name is your 2nd choice?
Insert letter of 2nd choice __________
5) Do you have any new suggestions for a class name category description?
a)__________
b)__________
c)_________ |
29. WHAT DO THESE FINDINGS MEAN?
Examined in combination, clinical trials have also provided evidence of
the dubious effectiveness of ‘new generation’ antidepressants.
In 2008 Irving Kirsch and co-authors published in the public
access journal, PloS Medicine a study entitled ‘Initial Severity
and Antidepressant Benefits: A Meta-Analysis of Data Submitted to the
Food and Drug Administration’. The journal editor’s summary of the
findings of Kirsch et al. tells the story:
These findings suggest
that, compared with placebo, the new-generation antidepressants do not
produce clinically significant improvements in depression in patients
who initially have moderate or even very severe depression, but show
significant effects only in the most severely depressed patients.
The
findings also show that the effect for these patients seems to be due
to decreased responsiveness to placebo, rather than increased
responsiveness to medication. Given these results, the researchers
conclude that there is little reason to prescribe new-generation
antidepressant medications to any but the most severely depressed
patients unless alternative treatments have been ineffective. In
addition, the finding that extremely depressed patients are less
responsive to placebo than less severely depressed patients but have
similar responses to antidepressants is a potentially important insight
into how patients with depression respond to antidepressants and
placebos that should be investigated further.
The complete paper can be accessed at:
http://medicine.plosjournals.org/perlserv/?request=get-document&doi=10.1371/journal.pmed.0050045#journal-pmed-0050045-g001
http://www.ahrp.org/risks/healy/FDA0204.php
http://www.ahrp.org/risks/healy/FDA0204.php
30. ATYPICAL ANTIPSYCHOTICS
Following the introduction of the 'atypicals' in 1997, suicide
numbers and rates rose by about 9% from 1996 to 1997, a large increase
although less than the 14% increase in the number of suicide
registrations. Hanging suddenly became the dominant means for suicide.
Hanging suddenly became the most popular means of suicide in akathisia.
http://www.nisu.flinders.edu.au/pubs/bulletin23/bulletin23-3.html
The trials of new generation or atypical antipsychotics that were
presented to the US FDA to get the 'atypicals' licensed yielded the
following outcomes: Zyprexa and Risperdal were twice as suicidogenic as
the antidepressants.
Drug |
Patient No. |
Suicides |
Suicidal Acts |
Risperdal |
2607 |
9 |
43 |
Comparator |
601 |
1 |
5 |
Placebo |
195 |
0 |
1 |
Zyprexa |
2500 |
12 |
Not disclosed |
Comparator |
810 |
1 (2) |
Not disclosed |
Placebo |
236 |
0 (1) |
Not disclosed |
Seroquel |
2523 |
1 |
4 |
Comparator |
426 |
0 |
2 |
Placebo |
206 |
0 |
0 |
Sertindole |
2194 |
5 |
20 |
Comparator |
632 |
0 |
2 |
Placebo |
290 |
0 |
1 |
Geodon/zisapride |
2993 |
6 |
Not disclosed |
Comparator |
951 |
Not disclosed |
Not disclosed |
Placebo |
424 |
0 |
Not disclosed |
|
31. ZYPREXA
This
was published by David Healy, after court-ordered access to Eli Lilly's
archives. No documentation of suicide attempts exists. We know only of
67 Zyprexa overdoses, and we know of those only if we read US Product
Information.
http://en.wikipedia.org/wiki/David_Healy_(psychiatrist)
These problems are documented in ZYPREXA PRODUCT INFORMATION (the US
version below). Reports of these overdoses, which are probably only
some of the suicide attempts, do not appear in Australian product
information nor in any information given to prescribers and patients,
nor, it seems, to those who write guidelines for the treatment of
schizophrenia.
Full prescribing information, including a boxed warning, is available at http://pi.lilly.com/us/zyprexa-pi.pdf
Experts
say it would be highly unlikely that a competent psychiatrist could
misdiagnosis this condition because the symptoms are so extreme and
distinct.
Once a drug is approved to treat one
condition, it is legal for doctors to prescribe the drug for other
uses. These unapproved uses are referred to as "off-label," and can
mean prescribing a drug for a longer duration than specified, at a
different dose, in combination with other drugs, or with a different
patient population than listed on the label.
http://www.tehachapinews.com/home/Blog/ZyprexaNews/17408
In reality, the atypicals entered the market with significant warnings
and are evolving a side effect profile that includes serious and life
threatening conditions in an alarming number of patients. In fact, the
FDA data established that one in every 145 persons enrolled in clinical
trials for these drugs died as a result of adverse reactions to the
drugs.
Independent researcher Dr. David Healy studied FDA raw data on the
atypical schizophrenia drug Zyprexa and concluded that it was among
“the deadliest drugs ever to gain FDA approval."
http://www.fda.gov/cder/foi/label/2004/20592se1-019_zyprexa_lbl.pdf
The FDA has issued an advisory about an increase of 70% in sudden death
in the demented elderly, and about a 70% increase in death in persons
over 60 on atypical antipsychotics.
32. FDA PUBLIC HEALTH ADVISORY DEATHS WITH ANTIPSYCHOTICS IN ELDERLY PATIENTS WITH BEHAVIOURAL DISTURBANCES
The
Food and Drug Administration has determined that the treatment of
behavioural disorders in elderly patients with dementia with atypical
(second generation) antipsychotic medications is associated with
increased mortality. Of a total of seventeen placebo controlled trials
performed with olanzapine (Zyprexa), aripiprazole (Abilify),
risperidone (Risperdal), or quetiapine (Seroquel) in elderly demented
patients with behavioural disorders, fifteen showed numerical increases
in mortality in the drug-treated group compared to the placebo-treated
patients. These studies enrolled a total of 5106 patients, and several
analyses have demonstrated an approximately 1.6-1.7 fold increase in
mortality in these studies. Examination of the specific causes of these
deaths revealed that most were either due to heart related events
(e.g., heart failure, sudden death) or infections (mostly pneumonia).
Date created: April 11 2005.
http://www.fda.gov/cder/drug/advisory/antipsychotics.htm
The US FDA was already aware of the death rates in clinical trials where 1 in every 145 clinical trial subjects died.
#
In the face of Eli Lilly failing to record suicide attempts, US Zyprexa
Product Information discloses that 67 persons out of 3,100 took
overdoses of Zyprexa and only one died. Eli Lilly argues the drug is
safe, because it is safe in overdose. Only 1 in 67 died. A
toxicologist's view would be appreciated here.
3100 was
number of subjects left in five trials presented to the US FDA after
two thirds had dropped out in less than six weeks, for reasons that
were never disclosed. One of the trials left was declared useless by
the US FDA, but it is used by Eli Lilly to produce information about
the 20 deaths See www.lillytrials.com
zyprexa_summary_917.pdf
zyprexa_summary_978.pdf
zyprexa_summary_980.pdf
zyprexa_summary_982.pdf
zyprexa_summary_1028.pdf
zyprexa_summary_1035a.pdf
zyprexa_summary_1035b.pdf
zyprexa_summary_1729.pdf
zyprexa_summary_1960.pdf
zyprexa_summary_2055.pdf
zyprexa _summary_2551.pdf
These original clinical trials which got Zyprexa licensed have now been
merged with hundreds of others on the Eli Lilly website.
This
product information does not disclose the causes of the overdosing, so
they could represent suicide attempts, akathisia or delirious
confusion.
For Dr. Grace Jackson's summary of these
trials, dropouts, suicides, FDA reviewer comments (but not eight
undisclosed deaths) see http://psychrights.org/states/Alaska/CaseOne/30-Day/ExhibitD-Olanzapine.htm
And a second current case in Alaska was settled in March 2008.
http://www.nytimes.com/2008/03/26/business/26cnd-zyprexa.html?_r=1&ref=business&oref=slogin
While
it seems to be about diabetes, it is fluctuations in blood sugar that
contribute to delirium and cause exacerbations of hallucinosis and
'schizophrenic reactions'. http://psychrights.org/States/Massachusetts/071006PsychRightsMassStrategyMemo.pdf
Fluctuating
blood sugar levels cause untoward behaviours. Perhaps more so when
combined with metabolites of Zyprexa and most if the drug in not able
to be metabolised so causes high blood levels, for genetic reasons, all
unrecognised.
The Montana case, alleging various forms of
fraud in the clinical trials that got the drug licensed and in its
later promotion, has been now joined by nine State Attorneys General.
http://www.helenair.com/extras/complaint.pdf
http://www.furiousseasons.com/legal%20documents/montanavlilly.pdf
http://www.furiousseasons.com/archives/2007/03/
the_zyprexa_chronicles_montana_alleges_kickbacks_and_offlabel_marketing.html
Concerns about safety and side effects are available at this infrequently accessed site: http://www.fda.gov/medwatch/SAFETY/2004/zyprexa_PI.pdf
Zyprexa product information contains this:
Body
as a Whole — Frequent: dental pain and flu syndrome; Infrequent:
abdomen enlarged, chills, face edema, intentional injury, malaise,
moniliasis, neck pain, neck rigidity, pelvic pain, photosensitivity
reaction, and suicide attempt;
Rare: chills and fever, hangover effect, and sudden death.
'Frequent' in drug company trial jargon is 1 in 10.
'Infrequent' lies somewhere between 1 in 10 and 1 in 500
Suicide
attempt is described as 'infrequent but none were ever disclosed.
According to David Healy, this data simply does not exist. (Personal
communication from Healy, who has examined the archive.)
'Rare'
is 1 in 500. Suicide is 'rare,' but catastrophic! Twelve persons out of
the remaining 2500 committed suicide (after two thirds of subjects had
dropped out). This is 1 in 208.
Sudden death is also described as 'rare' but there were eight deaths in about 7500 starters.
It would be well nigh impossible to get informed consent for a drug with that profile if safer alternatives were available.
5000
Zyprexa whistleblower documents about what Eli Lilly knew about
diabetes and other matters and what they did not disclose are now
available at:
http://www.furiousseasons.com/zyprexadocs.html
Allan Jones, the whistleblower whose testimony underpins litigation by
US State Attorneys General, against the Texas Medication Algorithm
Project (TMAP) a consortium that produced endorsements, protocols and
guidelines, writes:
In
reality, the 'atypicals' entered the market with significant warnings
and are evolving a side effect profile that includes serious and life
threatening conditions in an alarming number of patients. In fact, the
Food and Drug Administration (FDA) data established that one of every
145 persons enrolled in clinical trials for these drugs died as a
result of adverse reactions to the drugs. See this link
http://psychrights.org/index.htm
Also
http://tmap.wordpress.com/2008/02/25/nj-legislator-probe-antipsychotics-kids-medicaid/#more-69
33. THIS IS HOW THE FRAUD WAS PERPETRATED ON PSYCHIATRY:
Only
five Zyprexa schizophrenia trials were undertaken, but these generated
234 ghost-written articles by prominent “opinion leaders," which were
carefully placed in the prestigious journals, dependent for their
viability on pharmaceutical Industry advertising. The ghostwritten
articles and some algorithms for treatment emerged from the Texas
Medication Algorithm Project (TMAP), and their graphics bear a striking
resemblance to those on the TMAP website.
None of these
publications yielded any picture at all of the risk of suicide or
suicidal acts on these drugs, let alone sudden death.
“Endorsement science” has become the means of promotion.
The
colourful capsules appeared on the cover of Time, in The Washington
Times and The New York Times. The earlier drug company invention, the
“Dopamine Theory of Schizophrenia” was alive and well in these
endorsements, although by the time they were published it had no more
scientific validity than the serotonin theory of depression.
http://en.wikipedia.org/wiki/Texas_Medication_Algorithm_Project
Perhaps we need to laugh:
http://www.google.com.au/search?hl=en&q=fukitol&btnG=Google+Search&meta
Did anyone licensing this drug consider how side effects at this rate
might play out in the community? Placebo beats it every time.
And
What
these unrecognised side effects would cost the public purse? That is an
overdose rate of 2160 per 100,000, which is an awful lot of overdoses
given how many persons take olanzapine for the drug to gross to Eli
Lilly six billion dollars annually.
But overdose is not the preferred mode of suicide in akathisia, where suicides tend to be violent.
34. MANY MORE STUDIES CAN BE DOWNLOADED FROM
http://psychrights.org/Research/Dgest/AntiDepressants/AntiDepressants.htm
In
my study on an admission ward in 2003 and 2004, 161 persons came in
suicidal and a further with 40 diagnosed with akathisia and aggression;
44 came in suicidal, with akathisia and/or homicidal on olanzapine but
not olanzapine alone. That is a lot of pressure on beds. This is
similar to the situation in patients seen for other jurisdictions.
If these drugs behave in the community as they did in clinical trials, a public health problem is the inevitable outcome.
More information is accessed by the following links:
http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=193979
http://www.breggin.com/31-49.pdf
http://apt.rcpsych.org/cgi/content/full/12/5/320
http://www.bmj.com/cgi/content/abstract/330/7488/396
35. WHY ARE CLINICAL TRIALS IMPORTANT?
The clinical trials presented to the US FDA were a harbinger of what
might be expected if these drugs were released into the community.
In the community no raters familiar with side effects are employed, and
drugs are co-prescribed and compete for metabolic pathways, causing a
logjam at the liver as toxic metabolites recirculate and cause
symptoms.
36. WHY ARE PUBLIC HEALTH ADVISORIES SIGNIFICANT?
Public Health Advisories have been published by the US FDA regularly since 2003. These can be accessed by the link:
http://www.fda.gov/cder/drug/antidepressants/historical.htm
On
March 22, 2004, after a great deal of research, the FDA issued its
first Public Health Advisory about antidepressants for adults.
Adults
being treated with antidepressant medications, particularly those being
treated for depression should be watched closely for worsening of
depression and for increased suicidal thinking or behaviour. Close
watching may be especially important early in treatment, or when the
dose is changed, either increased or decreased. Adults whose symptoms
worsen while being treated with antidepressant drugs, including an
increase in suicidal thinking or behaviour, should be evaluated by
their health care professional.
The agency is also
advising that these patients be observed for certain behaviours that
are known to be associated with these drugs, such as anxiety,
agitation, panic attacks, insomnia, irritability, hostility,
impulsivity, akathisia (severe restlessness), hypomania and mania, and
that physicians be particularly vigilant in patients who may have
bipolar disorder.
http://www.fda.gov/cder/drug/antidepressants/PI_template.pdf
This
is not bipolar disorder. Manic shift occurs in persons using
antidepressants up to 30 times more often than could in bipolar illness
by chance. It remits when the drug is withdrawn. Manic shift
caused by antidepressant or other medication does not respond to
remedies for real, endogenous bipolar illness. Unstable moods
characterised by brief periods of energy followed by fatigue that
‘ropes you to the bed’, get worse and more and more drugs are
co-prescribed to deal with each side effect as if it was the condition
it suggested or mimicked.
http://ajp.psychiatryonline.org/cgi/content/full/165/3/300
This condition, legitimated by DSM, appears to be new and iatrogenic.
In psychiatry, organic brain syndrome mimics every disorder, just as neurosyphilis imitated all of them.
However,
a group of antidepressants that have worsening depression and
suicidality among their side effects may well explain the need for
scores of mood disorder specialists. If the first three
antidepressants tried by the GP did not work, then the fourth to the
eighth can be tried then 'augmented' with lithium, atypicals or thyroid
supplements, none of which has been shown to be effective.
http://www.breggin.com/31-49.pdf
Moreover
one cannot diagnose a ‘manic episode’ within criteria set by DSM or the
International Classification of Diseases if the symptoms are not due to
the direct physiological effects of a substance (e.g., a drug of abuse,
a medication, or other treatment) or a general medical condition (e.g.
hyperthyroidism).
From DSM IV:
Note:
Manic-like episodes that are clearly caused by somatic antidepressant
treatment (e.g., medication, electroconvulsive therapy, light therapy)
should not count toward a diagnosis of bipolar disorder.
So psychiatry invents a new category, Bipolar 11 for an
iatrogenic disorder, a toxic psychosis, and this leads to its treatment
by more medicines.
A list of drugs to be included in updated Public Heath Advisories can be found at:
http://www.fda.gov/cder/drug/antidepressants/antidepressantList.htm
The
problem in Australia is that the Adverse Drug Reactions Advisory
Committee (ADRAC) issued a belated and watered down advisory on August
4, 2005, only on its website, but it has not enforced its circulation
by the manufacturers to doctors.
http://www.tga.gov.au/adr/aadrb/aadr0508.htm#1
The
matter of the drug companies failing to disclose lethal side effects
may be a matter for the Commonwealth Attorney General. For example,
what Eli Lilly knew from 1978 but failed to disclose about its
antidepressant Prozac is well documented and can be accessed by the
link:
http://www.baumhedlundlaw.com/media/timeline.html
It
may be the case that fraud has been committed on the Commonwealth of
Australia as it has been on people and prescribers of the United
States. Here are some links to that information.
http://www.nytimes.com/2008/01/30/business/30cnd-drug.html?hp
http://www.mindfreedom.org/kb/psych-drug-corp/tmap/Texas-vs-TMAP-drug-fraud/
http://www.ahrp.org/cms/index2.php?option=com_content&do_pdf=1&id=411
The UK Healthcare Commission, faced with similar problems, called in
more relevant experts, pharmacists, who found that 70% of drugs given
to mental health patients had been poorly prescribed.
The Commission's report found that when pharmacists
reviewed patients' medications, 70 percent of cases resulted in a
change in the patient's medication, while 46 percent of patients whose
medication was reviewed were found to be taking their doses improperly.
The link to the news item is
http://www.naturalnews.com/021470.html
It is likely that biology accounts for massive dropout rates in clinical trials for both SSRIs and atypicals.
Up
to 75% do not complete the trials. Others have Valium co-prescribed and
the public is not told. Statistics about those who could not tolerate
drugs do not appear in product information.
If
people cannot metabolise the drug, its level in the rises and adverse
events follow. Some people do not get nausea, a useful early warning,
but quickly develop akathisia and psychosis. Such people might reject
their medication at home, but in hospital, one finds nurses and doctors
who urge patients to keep taking medicines – which, they should
realise, are making the patient sick.
Not all cytochromes can be induced. Some can be induced, but it does not happen overnight.
If
a person does not have the cytochromes to break down drugs, its
metabolites build up, and recirculate and produce a traffic jam at the
liver.
That’s why, when prescribing an SSRI or one
of the many other drugs, which are similarly metabolised, you ‘start
low – go slow’. Then ‘tolerance’ has a chance to develop and the drug
is better tolerated, and it might be more usefully used with impunity.
Toxins slowly ‘induce’ the enzymes that metabolise them, and in time
the liver is able to deal with higher doses. See the detailed answer
that has been provided to the question “Are there any antidepressive
medications that can be used by a poor metabolizer of the P-450 drugs?”
(Link below). For example, it’s stated:
There
is no reason why antidepressants can't be used in slow metabolizers –
you just have to be very, very careful. Beginning with very small doses
and measuring blood levels of the drug in question is appropriate. It
is also important to avoid co-administration of other drugs metabolised
by the same CYP enzyme.
http://www.healthieryou.com/mhexpert/exp1090202c.html
Many non-metabolisers can be identified through taking a good
medication history, starting low, adjusting the dose slowly, watching
and warning and, if necessary, not giving the same or similarly
metabolised drugs again.
http://findarticles.com/p/articles/mi_m0ISW/is_245/ai_111496944
http://www.healthanddna.com/drugreactiontest.html
Litigation
on the basis of being a non-metaboliser would be settled by the drug
company, as all of them have failed to warn of this vulnerable
population. As Eli Lilly failed to disclose information they had about
Zyprexa/olanzapine.
http://www.lawyersandsettlements.com/features/zyprexa-labels.html
6 US states have sued Janssen regarding Risperdal: Arkansas, Louisiana, Montana, South Carolina, Texas and Pennsylvania.
3 US states have sued Austrazeneca regarding Seroquel: Montana, Pennsylvania, South Carolina
At least 8 US states have sued TMAP over anti-depressants and antipsychotics and some ADHD medications.
Nine
US States have sued Eli Lilly regarding Zyprexa - Alaska, Louisiana,
Mississippi, Montana, New Mexico, Pennsylvania, South Carolina, Utah
and West Virginia.
The State of Connecticut has filed a
detailed statement of claim against Eli Lilly for various forms of
fraud in relation to the promotion of Zyprexa.
http://www.reuters.com/article/rbssHealthcareNews/idUSN1160916520080311?pageNumber=2&virtualBrandChannel=0
According
to the Connecticut complaint and in my own knowledge and experience in
Australia as well as in the United States, Eli Lilly's illegal
marketing enterprises and schemes included the following:
PEER-SELLING ENTERPRISE:
Lilly compensated medical marketing firms and several physicians who
routinely promoted Zyprexa to peer physicians in venues nationwide.
Physicians who attended "educational" events were deceived into
thinking that the events were independent of Eli Lilly. Conspiring
physicians concealed information about the efficacy of Zyprexa in
off-label uses and dangerous side effects, as well as the doctors'
financial ties with Eli Lilly.
THE ROLE OF PHARMACIES:
PUBLICATION ENTERPRISE:
Eli Lilly created a "Publication Enterprise" that hired writers to
create articles, and then paid specialists to "author" the articles.
The articles only included favorable results of Eli Lilly's own
internal trials, and suppressed unfavorable results, including a
clinical trial that failed to show Zyprexa's efficacy for bipolar
disorder.
PUBLIC PAYER ENTERPRISE: Eli Lilly
targeted those who oversaw treatment for people with serious mental
illness, including patients in mental hospitals and clinics who are on
Medicaid - among the largest users of antipsychotic drugs. Lilly also
influenced prescribing physicians to over-medicate senior citizens in
nursing homes and adolescents in detention centers with antipsychotic.
View the entire Lilly complaint from Connecticut
http://www.ct.gov/ag/lib/ag/health/elililly-zyprexa.pdf
And
see how Lilly promoted in Australia and by whom and for a general idea
of the level of support given to various researchers.
http://www.google.com.au/search?hl=en&q=Tim+Lambert+eli+lilly&btnG=Google+Search&meta
http://www.google.com.au/search?num=100&hl=en&q=Graham+Burrows+Eli+Lilly&btnG=Search&meta
The drug companies get away with it in Australia and psychiatrists (through peer reviews) help them.
Similar litigation about can be found at
http://www.google.com.au/search?num=100&hl=en&q=prozac+death+2000+vickery&btnG=Search&meta
37. HOW DOES THIS TRANSLATE INTO A PUBLIC HEALTH PROBLEM?
Many
drugs cross into the brain and have psychiatric effects, which are
often undesirable ones. One undesirable outcome might occur in the
treatment of genuine mental illness, when the patient becomes toxic on
medication, the doctor fails to recognise.
Genuine mental
illness, such as bipolar disorder, biological depression or
schizophrenia, might have been present in the patient before taking the
medication. But that medication might have had hallucinations, mania,
delusions or schizophreniform reaction among its side effects. And in
the case of risperidone, 6 manic reactions on placebo and 8 on active
substance. And this drug is licensed to treat mania? It
increases the risk of it. See old Risperdal Product information:
Table
2. Incidence of Treatment-Emergent Adverse Events in a 3-Week,
Placebo-Controlled Trial - Monotherapy in Bipolar Mania Body System/
RISPERDAL® Placebo Preferred Term (N=134) (N=125)
Central & peripheral nervous system
|
Risperdal |
Placebo |
Dystonia |
18% |
6% |
Akathisia |
16% |
6% |
Dizziness |
11% |
9% |
Parkinsonism |
6% |
3% |
Hypoesthesia |
2% |
1% |
Psychiatric
Somnolence |
28% |
7% |
Agitation |
8% |
6% |
Manic reaction |
8% |
6% |
Anxiety |
4% |
2% |
Concentration impaired |
2% |
1% |
This information has been eliminated from the latest PI. Akathisia is eliminated altogether in the latest version.
http://www.risperdal.com/risperdal/shared/pi/risperdal.pdf
It is necessary to investigate the original diagnosis and question
whether these disorders were not present before medication was started.
If the disorders weren’t present, then the patient is very likely to be
misdiagnosed and that patient may well be part of the new, second 50%
of the treatment-seeking population.
38. SEVERAL PATHWAYS TO CHRONIC INVALIDITY
There
must be causes for an epidemic of mental illness to come about. First
the drugs do not work in a lot of people, and second their side effects
are being misdiagnosed as mental illness and they are given more drugs
that do not work. This problem has a number of starting points.
- A hallucination has been caused by a street drug: strong cannabis, speed or another.
- The
initial 'psychiatric' symptom is a side effect of a non-psychiatric
medication such as an anti-emetic, calcium channel blocker,
antimalarial, antihistamine, conjugated oestrogen, triptan, Tramadol,
or any one of five hundred drugs listed as causing psychiatric side
effects or Serotonin Syndrome in some people. Serotonin Syndrome
causes confusion, delirium with hallucinations, mania, depression or an
organic schizophreniform disorder.
- These might not
be recognised as side effects and so they are treated with an atypical
antipsychotic or an antidepressant that has the same psychiatric
symptoms among its reported side effects.
- New
generation or 'SSRI' antidepressants prescribed for stress, grief,
girlfriend trouble, menopause and anxiety, any human events, boyfriend
trouble, and they cause some people to become suicidal, hallucinated
and aggressive. This side effect is mistaken for depression, mania,
schizophrenia, or if it persists, for borderline personalty disorder.
- A
patient on antidepressants or atypical antipsychotics becomes manic and
is then gets diagnosed as bipolar. But as this is neurotoxic, it does
not respond to the remedies for true bipolar, so they do not recover.
- A depressed patient gets worse, hallucinated or suicidal, so is prescribed more medication.
- Patients
with schizotypal personality disorder (which affects 3% of the
population) are at risk of being misdiagnosed as schizophrenic. They
may then be medicated with drugs that induce schizophreniform symptoms,
delusions and hallucinations and they then are sometimes forcibly
medicated with more psychiatric medication. They are given new
schizophrenia medicines, one or more of Zyprexa, Risperdal or Seroquel,
in series or in parallel, and no one improves. This is because one is
treating not schizophrenia but a toxic mimic of schizophrenia and
treating a side effect with another similar toxin, which cannot be
easily metabolised.
- Then more medications are added, different ones in each case.
- Drugs
marketed as 'mood stabilisers' that have no such effect, more
antidepressants, more antipsychotics, sleeping pills, sedatives,
benzodiazepines as well as antiemetics for nausea, remedies for
diarrhoea and antihypertensives for high blood pressure. Mood
stabilisers are added to mood de-stabilisers and new disorders emerge
from that.
- A list of drugs that inhibit CYP450 2D6
includes amphetamines. Poor tolerance of amphetamines suggests
that a person might be a poor or intermediate metaboliser and is at
risk of responding adversely to other meds that require 2D6 and even
more adversely when they are drugs (or are combined with drugs) that
inhibit 2D6 because they effectively turn intermediated metabolisers
into poor metabolisers. Similarly if a person had already
responded poorly to drugs that require 2D6, it seems not to be a good
idea to give them other drugs that require the same metabolic pathway,
singly or in combination. 2D6 is a non-inducible enzyme, which is
virtually absent in 8% of Caucasian and there is a 100% variance
between individuals in the same population, in that some are ultrarapid
metabolisers. This is all in MIMS ANNUAL but not in what drug
reps pass out. So it is not the doctors' fault and patient in USA
sue the drug company successfully for failing to reveal this
information, which they had in their possession forever. They fail to
reveal it for commercial reasons and these problems are now coming home
to roost in the form of litigation by state attorneys and individuals
as well as class actions.
As
the rate of bipolar rose in USA and Australia, the DSM invented more
catef gories to deal with this new epidemic without losing patients.
A
century ago, rapid-cycling bipolar disorder was not observed. Either
classic nosologists, such as Kraepelin, simply missed it or it did not
exist. The term was first coined in the 1970s to identify lithium
nonresponders in randomized clinical trials; thereafter, rapid cycling
became the subject of decades of further research, which has confirmed
that rapid cycling is a factor in poor prognosis. Rapid-cycling
patients do worse in follow-up than patients without rapid cycling, and
they are also less likely to respond to treatment. The erroneous
impression then arose that anticonvulsants, such as carbamazepine or
divalproex, were more effective than lithium in treating rapid cycling.
The error came from comparing studies using lithium alone against
studies using anticonvulsants alone, without a direct comparison of the
two treatments. Such comparisons need to be made head to head, in
randomized studies. When these comparisons are performed with proper
methods, anticonvulsants are seen to be about equivalent to lithium
(i.e., ineffective) in treating rapid cycling (1, 2).
http://ajp.psychiatryonline.org/cgi/content/full/165/3/300
In
bipolar disorder, one often has to wonder if it is medication-induced
bipolar that is causing the problems, because the condition simply does
not get better.
But aside from these hazards, there are
also grounds to question whether the treatment effects that some think
have been demonstrated in bipolar disorder trials translate into
therapeutic efficacy.
If use of these agents based on
demonstrated effects leads on to efficacy, admissions for bipolar
disorder might be expected to fall, but the evidence for this is
difficult to find.
In North Wales before the advent of
modern pharmacotherapy, patients with bipolar I disorder had on average
four admissions every ten years. In contrast, against a background of a
constant incidence of bipolar I disorder, and dramatic improvements in
service provision, bipolar I patients show a 4-fold increase in the
prevalence of admissions despite being treated with the very latest
psychotropic medications. This is not ordinarily what happens when
treatments “work,” but quite often is what happens when treatments have
effects.
From
http://medicine.plosjournals.org/perlserv?request=get-document&doi=10.1371/journal.pmed.0030185
39. SEVERAL PATHWAYS TO CHRONIC INVALIDITY
Sedatives,
benzodiazepines may be added to the mix, as well as sleeping pills, in
the face of product information that antidepressants enhance and
prolong their sedative and confusional effects
Benzodiazepines.
The half-life of concurrently administered diazepam may be prolonged in
some patients ...Co-administration of alprazolam and fluoxetine has
resulted in increased alprazolam plasma concentrations and in further
psychomotor performance decrement due to increased alprazolam levels.
Then second and third 'antipsychotics' are
administered, so by the time they come into hospital they are taking
between one and five drugs. By then they're also on medications for nausea and
diarrhoea, Stemetil and Losec, both of which have interactions with
what is already present.
Each drug was prescribed as an
antidote to a side effect. All put stress on the CYP450 metabolic
pathways. This is all in MIMS Annual, but not honoured in the
observance. A first-rate tutorial and charts can be found at www.genelex.com
Good
history taking will reveal whaUsing 'patient exposure years' and
combining suicides in withdrawal from drugs in use, Khan reported a
rate 752 per 100,000 persons for those treated with atypical
antipsychotics--risperidone, olanzapine, and quetiapine; Among 10,118
participating patients, in antipsychotic trials presented to the US FDA
26 committed suicide and 51 attempted suicide.
Using similar criteria he examined Food and Drug Administration (FDA)
summary reports of the controlled clinical trials for nine modern
FDA-approved antidepressants provided data for comparing rates of
suicide and found that of 48,277 depressed patients participating in
the trials, 77 committed suicide.
This was a rate 718 per 100, 000 persons for those treated with selective serotonin reuptake inhibitors;
Khan
also reported a suicide attempt rate of 4% in clinical trial subjects
of antidepressants after 10-week trials. He noted that suicidal
persons and those carrying suicide risk had not been allowed to become
clinical trial subjects. These drugs were targeted at lesser
'ills,' stress, unhappiness and social anxiety and clinical trial
subjects had those conditions and had become suicidal on use and after
use, in withdrawal and in the year following.
This is 4000 per 1000,000, an enormous rate, with enormous public health consequences.
Some are left with neuroleptic-induced deficit syndrome (NIDS) and may be permanently damaged.
http://psychrights.org/Drugs/DrJacksonUCELecture(UK)09.06.04.pdf
http://www.ncbi.nlm.nih.gov/sites/entrez?db=pubmed&cmd=Search&Term=NIDS%20neuroleptic&itool=QuerySuggestion
40. WHAT IS AKATHISIA AND HOW DOES IT DIFFER FROM SCHIZOPHRENIA?
Completed
suicide is the measurable tip of poorly recognised psychotropic side
effects, which have been systematically and deliberately discounted as
‘the patients’ problems’. Pharmaceutical companies lose no opportunity
to belittle David Healy, who was able through court orders to prise
clinical trial statistics out of the FDA, and Peter Breggin, who was
the first to bring to public notice the risks of new antidepressants
and other medicines used for psychiatric purposes. Breggin defined a stimulant continuum beginning with lesser
degrees of insomnia, nervousness, anxiety, hyperactivity and
irritability, which progresses toward more severe agitation,
restlessness, aggression and varying degrees of mania. Mania or
manic-like symptoms include disinhibition, grandiosity; sleep
disturbances and out-of-control aggressive behaviour. The patients
cycle into depression and suicidality. They can produce a combined
state of stimulation and depression, an agitated depression, with a
high risk of suicide and violence. Panic and anxiety are common.
http://www.breggin.com/31-49.pdf
Obsessive
preoccupations with aggression, against self or others, are often
accompanied by a worsening of any pre-existing depression. Depression
and suicidality may appear in persons treated for anxiety or other
disorders. A state similar to personality disorder with borderline
traits may appear in mature, formerly stable persons. Its extreme
results from a combination with alcohol and substance abuse, in what
seems to be an attempt to relieve the ‘living hell’ that the worst and
most dangerous side effect, akathisia, creates. Akathisia may present as a diffuse psychomotor restlessness,
which affects the patient’s entire body, an increased tenseness,
insomnia and a feeling of being very uncomfortable, frequently
verbalised, as "I don’t feel like myself, weird, strange, not me."
Patients feel they are going mad, in turmoil, and numb as if nothing
matters. Embarrassed, they do not confess their impulses. Eliciting
them needs careful questioning. These experiences can go on for hours
or years, or can be acted on very quickly, in a matter of minutes.
I repeat:
Acute akathisia is a psychiatric emergency. Recurrent episodes
of hallucinatory delirium along violent or sexual themes with colourful
visual, voice and tactile hallucinations may be misdiagnosed as a
schizophrenic illness. Sexual craving has been reported.
Akathisia
has a strong association with violence, self-harm, suicide and
homicide. It is an inner restlessness or jitteriness, accompanied by a
subjective as well as objective compulsion to move, abscond, pace or
run, or drive long distances in a somewhat dissociated state. Akathisia
can lead to suicide because it is intolerable. Intense and involuntary
preoccupation with unwelcome, obsessively violent thoughts is
pathognomonic.
A pathognomonic sign or symptoms is a particular sign whose presence
means, beyond any doubt, that a particular disease is present. It is
derived from the Greek páthos (πάθος, disease) and gnōmon (γνώμον, "judge"). Labelling a sign or symptom "pathognomonic" represents a marked intensification of a "diagnostic" sign or symptom.
First recognised in users of reserpine for high blood pressure,
akathisia and suicide became prominent in the forensic literature of
the 1970s and 1980s as an effect of haloperidol and, later, of
flupenthixol.
The
above syndromes often appear in combination with each other. They may
recede within days of stopping the medication or persist, requiring
hospitalisation and additional treatment over subsequent weeks or
months. They occur in individuals with no prior history of violence,
suicidality, psychomotor agitation or manic-like symptoms. Some
patients cannot easily stop taking these medicines without going into a
state of withdrawal. They are, technically, addicted.
No single word describes the problem. Dr. Ken Gillman proposes 'toxidrome'.
http://www.psychotropical.com/
My preference is for ‘neurotoxicity spectrum disorder’ to describe the
manifestations of intoxication with medications said to have
serotonergic and/or dopaminergic properties.
Professor Perminder Sachdev has proposed a classification of one of these, akathisia.
http://www.psychrights.org/Articles/EHPPPsychDrugEpidemic(Whitaker).PDF
Since
1994, SSRI-induced akathisia has been recognised in the Diagnostic and
Statistical Manual (DSM IV TR), where it is coded as a movement
disorder, but it fits equally well into drug-induced psychotic states
or with organic brain syndromes. A useful concept is the “akathisia-prone patient”: one who is
likely to develop akathisia on tricyclics, lithium, SSRIs, Zyprexa,
Risperdal, Solian and Seroquel (quetiapine) as well as a variety of
other medications (often Lipitor and conjugated oestrogens,
antihistamines, antiemetics and calcium channel blockers). Akathisia
accompanies the taking of the medication but it can also occur if a
drug is stopped suddenly rather than slowly. Many suicides and
homicides are committed in withdrawal, which can go on for three months
in some circumstances.
It should not surprise anyone
to find that psychotropic drugs have psychiatric side effects, but they
are poorly recognised as such, even by psychiatrists, because they
occur in the context of treatment for ‘psychiatric’ conditions.
Sublethal side effects place heavy demands on mental health resources.
It is rare to see a person who has been on these medicines for some
time who is not also taking co-prescribed tranquillisers of one kind or
another.
Suicide is an indicator of how neurotoxic a
medication is. In February 2008, the FDA undertook to pay attention to
suicidality in future clinical trials of all medicines, and not before
time.
Descriptions of akathisia abound in medical and legal literature.
http://en.wikipedia.org/wiki/Akathisia
http://www.antidepressantsfacts.com/Akathisia%20as%20Violence.htm
http://www.antidepressantsfacts.com/akathisia-mania.htm
http://www.lawyersandsettlements.com/features/ssri-suicide-akathisia.html
http://www.jeffmann.net/NeuroGuidemaps/akathisia.html
In Australian a legal case of akathisia in its acute form (homicidal
and suicidal) is well described in R v Hawkins Supreme Court of NSW
2001. The link is:
http://www.austlii.edu.au/cgi-bin/sinodisp/au/cases/nsw/NSWSC/2001/420.html?query=akathisia
Akathisia
in its chronic form (also homicidal and suicidal) is well described in
R v B Supreme Court of WA 2004, in the sentencing judgement in R v B
SCWA 67 of 2004.
Richard Guilliatt reported on "B" in the Sydney Morning Herald’s Good Weekend on May 19, 2004:
http://theeffexoractivist.org/forum/viewtopic.php?t=891&sid=9a4ed8c52d980799e5cdc8026c02884a
A
search for akathisia through Austlii, (the legal database) repeated
using ‘law’ through Google, throws up literally hundreds of
well-described cases through the links below http://www.google.com/search?q=akathisia+(law+OR+legal+OR+legislation+OR+regulation+OR+judgment+OR+treaty)
Rebekah Beddoe’s story as told in her book ‘Dying for a Cure’ has
already been detailed. Ms Beddoe discovered on the Internet how
to slowly withdraw herself from the medicines and she did so. She had
endured many hospitalisations and had developed diabetes on
Zyprexa/olanzapine, a Special Purpose medication licensed for
schizophrenia alone.
She did not have schizophrenia at all. She had side effects, which
disappeared when she stopped the antidepressant and all that had been
prescribed with it.
TIME
MAGAZINE published her story. That article is reproduced in full on one
of the many patient chat rooms, which brought the drug companies to
their knees:
http://www.time.com/time/pacific/mag...0228-1,00.html
http://www.time.com/time/magazine/article/0,9171,503051121-1130228-1,00.html
If Rebekh Beddoe's response to Zoloft only happened in 1-3% of users,
then SSRI side effects are already presenting the taxpayer with a
serious economic problem. In some studies, suicidal thinking and
behaviours on "SSRIs" have been noted at a rate of 27%.
In common among the many patients who comprise the increased numbers of
those seeking mental health care since 1992 is that they did not have
mental illness before they were given medication, which caused side
effects including suicidality, akathisia, aggression and hallucinations.
The Royal Australian and New Zealand College of Psychiatrists (RANZCP)
Clinical Practice Guidelines advocate the use of Efexor/venlafaxine,
stating
'Depression is common. In the Australian Mental Health Survey, 4% of adults had a depressive disorder in the past month.'
These guidelines can be accessed at the link below:
http://www.ranzcp.org/pdffiles/cpgs/Depression%20Clinican%20Full.pdf
The RANZCP recommend the use of Efexor/venlafaxine for such conditions.
People taking venlafaxine committed suicide at six times the rate of
those taking a placebo in the same trials. Each completed suicide
represents 20-40 attempts, some of which require hospital admission.
Efexor is as toxic as older antidepressants in overdose. This study
suggests that these drugs do more harm than good. The RANZCP should
arrange urgently for a pharmacologist and pharmacogeneticist to look
over its recommendations for treatment, as the epidemic spread and
intractability of depression demonstrates that there is something
wrong.
Product information, from the United States. on Effexor contains the following side effects:
Nervous system - Frequent: amnesia, confusion, depersonalization, hypesthesia, thinking abnormal, trismus, vertigo;
Infrequent:
akathisia, apathy, ataxia, circumoral paresthesia, CNS stimulation,
emotional lability, euphoria, hallucinations, hostility, hyperesthesia,
hyperkinesia, hypotonia, incoordination, manic reaction, myoclonus,
neuralgia, neuropathy, psychosis, seizure, abnormal speech, stupor,
suicidal ideation;
Rare: abnormal/changed behavior,
adjustment disorder, akinesia, alcohol abuse, aphasia, bradykinesia,
buccoglossal syndrome, cerebrovascular accident, feeling drunk, loss of
consciousness, delusions, dementia, dystonia, energy increased, facial
paralysis, abnormal gait, Guillain-Barre Syndrome, homicidal ideation,
hyperchlorhydria, hypokinesia, hysteria, impulse control difficulties,
libido increased, motion sickness, neuritis, nystagmus, paranoid
reaction, paresis, psychotic depression, reflexes decreased, reflexes
increased, torticollis.
And if you examine for them you will find them. Hence many homicides and mass homicides have occurred on Efexor.
http://www.bmj.com/cgi/content/abstract/334/7587/242
When challenged after the Hawkins case was decided (see earlier), this is what Professor Ellis wrote:
There
have been rare reports of fluoxetine and, more recently, paroxetine and
sertraline being associated with aggressive or suicidal thoughts and
behaviour. Due to similar pharmacological profiles, the same reactions
may occur with other selective serotonin re-uptake inhibitors (SSRIs).
It is possible that these reactions can be attributed to akathisia
(involuntary severe motor restlessness).
However, the most common reason for self-harm behaviour during
treatment with any antidepressant is worsening depression. The
development of severe agitation or self-harm behaviour is an indication
that the patient and their antidepressant therapy require prompt
review. Patients should be advised to seek medical attention as soon as
possible if they develop agitation or restlessness, or if their
depression worsens.
Reports of aggressive and suicidal behaviour with SSRIs investigated.
Behaviour change may be due to SSRI-induced akathisia. Agitation or
harmful behaviour signals need to review both patient and treatment
immediately.
Informing patients to seek help may help reduce adverse outcomes.
http://www.medsafe.govt.nz/Profs/PUarticles/SSRI.htm
Those
who attract pharmacological treatment under these guidelines would
mostly be ordinary people suffering normal human emotions that have
been relabelled as ‘depression'.
Campaigns to
treat depression have been so successful that there are now nearly a
million Australians, 200,000 of them children, taking antidepressants,
and many others have tried them. When the guidelines were criticised,
Professor Hickie told us: 'The guideline for the treatment of
depression makes sound recommendations, in agreement with comparable
guidelines from the US and the UK.'
All
had a common source, the Texas Medication Algorithm Project, TMAP, now
subject to fraud litigation, where drug companies had taken over
creating and writing guidelines.
http://en.wikipedia.org/wiki/Allen_Jones_%28whistleblower%29
41. HOW MANY BEDS DO SUCH PATIENTS OCCUPY?
I
made 190 reports to the Adverse Drug Reactions Committee (ADRAC) from
one inpatient unit and from 12 related (through treaters) medicolegal
reports during 2003 and 2004. I have since made a further 300
approximately from my compensation and criminal jurisdiction practice.
65
of the patients were taking Efexor/venlafaxine, which has suicidal
thinking and acts as well as homicidal ideation among its listed side
effects. Other drugs which were not available before 1992 were also
well represented. A surprise was the number of times that an older
injectable drug, Clopixol, which was not ever used on its own, caused
homicidal ideation and violence. However this number is meaningless
without knowing how many persons in that community were getting it.
The Department of Health refused to acknowledge that a public health problem existed.
http://www.bmj.com/cgi/content/abstract/334/7587/242
26 patients on various new drugs had made homicidal attacks. There are
now five suicides in this series. I warned in writing of dangerous
prescribing in 17 cases, and my warnings were inevitably followed by
'SSRI events', suicide attempts or violence.
Sweden acknowledges, investigates and reports this problem.
http://psychrights.org/Articles/SwedishSuicides.htm
Australian coroners use toxicologists as experts and most lack the
education and training to identify and investigate the issue of suicide
induction so the Minister is simply not told how bad the problem is in
Australia.
In
many cases, an "SSRI" generation antidepressant had been prescribed and
the patient had become suicidal, hallucinated and aggressive. The
patient’s condition was then mistakenly diagnosed as schizophrenia. All
were given new schizophrenia medicines, one or more of Zyprexa,
Risperdal or Seroquel, in series or in parallel, and not one improved.
Then more medications were added, different ones in each case: ‘mood
stabilisers', sedatives, sleeping pills and second and third
antipsychotics
Sometimes this march into chronic
psychiatric invalidity had started with a hallucination caused by a
non-psychiatric medication or street drug, which was treated with
another toxic atypical antipsychotic.
Such patients
made up about a third of admissions in one region, but at least half of
the workload, as they presented many times before being recognised, one
more than 30 times. They recovered when the causal medicines were
withdrawn, but some did eventually commit suicide.
Some
worked it out for themselves and stopped taking pills. Many were
discharged on the same medicines as had caused their admissions, and
some on increased doses with disastrous results.
Imagine this:
Panopticure is launched, a new drug for Glaucoma, a serious eye condition which, untreated, causes blindness.
Learned
professors, all over the world, publish strikingly similar papers to
the effect that the prevalence of Glaucoma, and its dire consequences,
has all been seriously underestimated. And that Glaucoma is serious,
treatable and affects four percent of the population every month.
Panopticure and its copycats boom.
And in Australia alone, some ten years later, it is not 100,000 patients under treatment for Glaucoma, but a million.
Drug representatives tout Panopticure for sore eyes, blurred vision, myopia, presbyopia, or simply to induce clear vision.
Reports
should start appearing in the literature that some users go blind – but
they are ignored. We are repeatedly reassured: It’s the disease, not
the drug, doctor.
In the United
States, litigators access drug company data, and find that clinical
trials had shown that some people being treated for sore eyes went
blind on Panopticure.
They find the
maker paid off officials of the US Food and Drug Administration and the
Office of Drug Safety did not examine clinical trial data that had not
been put in front of them.
The Bush Administration stifled Federal investigations into how this had occurred.
Panopticure
paid out millions in compensation as evidence was good and passed 6
Daubert hearings. The maker knew that in clinical trials one in 250
became permanently blind and many partially so. And this was after six
week trials from which two thirds of participants dropped out. They did
not tell us why they could not take the drops for six weeks.
Panopticure appeared on the front cover of American TIME MAGAZINE.
Ten
years after the introduction of Panopticure, the Department of health
told us that the number of persons on blind pensions had increased by
100%.
And by a further 25% in the next four years.
You would think that there would be an outcry – and that ophthalmologists collectively would be angry at being duped.
But psychiatrists do not seem to have the same concern or remain unaware of why they need more resources.
Few would believe these to be the intrinsic risks of transiently raised ocular pressure.
That 4% of us experience in each month. |
Yet
this is the composite tale of the drugs launched by the TEXAS
MEDICATION ALGORITHM PROJECT. George Bush was Governor of Texas.
RISPERDAL,
ZYPREXA, (Eli Lilly) SEROQUEL, LEXAPRO, (Novartis) CIPRAMIL, (Novartis)
ZOLOFT, AVANZA, ZYBAN, SERZONE, EFEXOR (Wyeth) and PROZAC. These are
called the ‘serotonin drugs’ as all boost serotonin. Their names
are the product of market research. TMAP’s ghostwriters influenced
RANZCP guidelines to depression, to schizophrenia, which are much the
same those used in beyondblue
and its subtended GP eduction programs. These guidelines tell us how to
treat depression with new miracle drugs. And how to treat their side
effects, their complications with atypical antipsychotics.
The Ghostwriters are (this information comes from David Healy)
Current Medical Directions http://www.cmdny.com
Whose remit is
“to deliver scientifically accurate information strategically developed for specific target audiences”
CMD
writes up studies, review articles, abstracts, journal supplements,
product monographs, expert commentaries and textbook chapters. It
conducts meta-analyses, and organizes journal supplements, satellite
symposia, and consensus conferences as well as advisory boards for its
clients
[CMD] “strives to exceed the expectations of our clients and to assist them in achieving their strategic objectives”.
Australia is lagging behind the rest of the world in addressing a problem first reported in the 1980s.
This is because (unlike its counterparts in Canada, the UK and the USA)
the various instrumentalities of the NSW Department of Health (Area
Health Services, the Health Care Complaints Commission) rely on peers
and collective opinion (consensus gentium, i.e of the people) of the
RANZCP rather than on research and cutting edge information when they
issue guidance and advisories to practitioners.
The NSW Department of Health relied on the collective opinion of the
Royal Australian and New Zealand College of Psychiatrists and did not
pass on the FDA Public Health Advisory: Worsening Depression and
Suicidality in Patients Being Treated With Antidepressants. March 22,
2004
http://www.fda.gov/CDER/Drug/antidepressants/AntidepressanstPHA.htm
The College spokesman, Dr. Bill Lyndon, responded to US FDA advisories in The Australian on 24 March 2004, saying
'We are not convinced.'
And later
But
we also need to be careful not to throw out very important drugs that
save a lot of lives on the basis of as yet unsubstantiated claims or
unproven claims.
The claims that new antidepressants caused suicides
at least double placebo were very well substantiated by March 24, 2004.
In June 2005, the US FDA conceded legal causation.
http://www.fda.gov/cder/drug/advisory/SSRI200507.htm
http://www.socialaudit.org.uk/58090-DH.htm
http://psychrights.org/expertestimony.htm
October 4, 2002, Ronald W. M. MARIS PhD, Distinguished Professor Emeritus, Maris@sc.edu, 803-777-6870, www.suicideexpert.com
ABSTRACT:
This paper critically examines several methodological issues growing
largely out of Daubert, pertinent to the question of whether or not
SSRI medications can be said scientifically to cause suicide ideation,
suicide attempts, and/or completed suicide.
http://www.lucire.com.au/documents/Maris_Daubert-Competent_Scientist.aspx
Background:
There has been a long-standing controversy about the possibility that
selective serotonin reuptake inhibitor (SSRI) antidepressants might
induce suicidality in some patients.
Methods:
Starting from the clinical studies that gave rise to this issue, this
paper reviews an unselected cohort of randomised clinical trials
(RCTs), a series of meta-analyses undertaken to investigate aspects of
the problem, studies in recurrent brief depressive disorders,
epidemiological studies and healthy volunteer studies using SSRIs to
shed light on this issue.
Results: The original
clinical studies produced evidence of a dose-dependent link, present on
a challenge, de-challenge and rechallenge basis, between SSRIs and both
agitation and suicidality. Meta-analyses of RCTs conducted around this
time indicate that SSRIs may reduce suicidal ideation in some patients.
These same RCTs, however, yield an excess of suicides and suicide
attempts on active treatments compared with placebos. This excess also
appears in the best-controlled epidemiological studies. Finally,
healthy volunteer studies give indications that SSRIs may induce
agitation and suicidality in some individuals.
Conclusions:
The data reviewed here, which indicate a possible doubling of the
relative risk of both suicides and suicide attempts on SSRIs compared
with older antidepressants or non-treatment, make it difficult to
sustain a null hypothesis, i.e. that SSRIs do not cause problems in
some individuals to whom they are given. Further studies or further
access to data are indicated to establish the magnitude of any risk and
the characteristics of patients who may be most at risk.
http://www.healyprozac.com/EditorsDilemma/Psychotherapy_Psychosomatics.pdf
http://www.abc.net.au/worldtoday/content/2004/s1073736.htm
There is no evidence that antidepressants save lives or reduce suicide in users.
The ADRAC Advisory of August 4, 2005, states
Increased
prescribing of antidepressants in Australia during 1991-2000 was
associated with decreasing suicide rates, with the trend being most
apparent in older age groups.
ADRAC cites Hall WD, Mant A, Mitchell PB, Rendle VA,
Hickie IB, McManus P. Association between antidepressant prescribing
and suicide in Australia, 1991-2000: trend analysis. BMJ
2003;326:1008-1.
http://www.bmj.com/cgi/content/full/326/7397/1008
However, the cited paper does not contain any such suggestion.
Suicide
rates in older age groups had been falling for some years, with
improved social services. Professor Hickie has often repeated what
ADRAC reported. The conclusion of the paper actually states:
Results:
While overall national rates of suicide did not fall significantly,
incidence decreased in older men and women and increased in younger
adults.
http://www.bmj.com/cgi/eletters/326/7397/1008
42. PROFESSOR IAN HICKIE, PSYCHIATRIST, ON CHANNEL 9 PROGRAMME SUNDAY 9TH MARCH, 2008
“I
would like to be quite blunt about it. From the large evidence
base that we have there is not systematic evidence of over-prescribing
in Australia. There is also clear cut evidence that increased
treatments for depression in Australia has resulted in decreased
suicides in Australia. So, more people treated, medicine, psychological
counselling, support – less dead people.”
Older antidepressants saved lives only in a small
high-risk population of persons with melancholic 'hospital' or
'biological' depression where the antidepressants could be carefully
administered and monitored.
The pharmaceutical
industry rewards opinion leaders who promote their drugs, as described
by Roy Moynihan in his acclaimed book, Selling Sickness.
http://www.bmj.com/cgi/content/full/324/7342/886
The pharmaceutical industry is allowed to help with mental heath
planning. Persons with benefits from the industry advise on mental
health policy.
The
NSW Health Care Complaints Commission is the only body available in the
state to consider treatment complaints, and it similarly relies on
peers of the prescribers, who are likely have the same knowledge
deficits as those who are the subject of treatment complaints.
The
HCCC was set up in 1993, in the wake of the Chelmsford Royal Commission
(1988-90) to ensure that malpractice of such magnitude could not recur.
26 deaths and suicides were occasioned by the pharmacological treatment
delivered by the late Dr Harry Bailey, Director from 1963 to 1979 of
the Neuropsychiatric Institute and later the Chelmsford Private
Hospital, a private psychiatric institution in Sydney.
It is somewhat ironic that reports of more preventable deaths and
suicides than Bailey ever caused in the same time frame have been
investigated and dismissed in a cavalier fashion by the Medical Board
of NSW. Its anonymous 'peer reviewers' find nothing suspicious about a
similar series of events, suicide attempts and suicide deaths, a
bleeding death when my tragic and alarming series was reported.
The cause, with Bailey's Chelmsford patients as well as those in the present time, was medication-induced akathisia.
Today's medicines produce more akathisia, (Zyprexa 27%) more have more
side effects and are given to more people than ever took psychotropic
medication in the 1970s. More reports were lodged at the US FDA
about Prozac than about any other drug http://www.oism.info/en/psychiatric_drugs/harm/fda_report_prozac_side_effects.htm drug in the history of the US FDA.
Further useful links can be found here:
http://www.lucire.com.au/documents/Links.aspx
And for fun and good measure, this one:
http://carlatpsychiatry.blogspot.com/2008/02/counter-detailing-for-kevin-md.html
Think of your own kids when you see how medications are being promoted for other kids.
http://en.epochtimes.com/tools/printer.asp?id=64187
43. HOW WE WERE ALL SNOWED BY BIG PHARMA.
The following books were reviewed by Quentin Crews in the New York Review of Books
The Loss of
Sadness: How Psychiatry Transformed Normal Sorrow into Depressive
Disorder by Allan V. Horwitz and Jerome C. Wakefield, Oxford University
Press, 287 pp., $29.95
Shyness: How Normal Behavior Became a Sickness by Christopher Lane, Yale University Press, 263 pp., $27.50
Let
Them Eat Prozac: The Unhealthy Relationship Between the Pharmaceutical
Industry and Depression by David Healy, New York University Press, 351
pp., $18.95 (paper)
See reviews
http://www.nybooks.com/articles/20851
I commend the Semmelweiss Organization.
http://www.semmelweis.org/Acrobat/article_uoworks_peer_review.pdf
Diamond and Kabul's insight that:
“When
the evidence conflicts with our judgment we tend to resist it, but when
the evidence is consistent with our judgment we tend to embrace it”
This phenomenon is well known to psychologists as confirmation bias.
It was also known to the ancients:
"When
a man finds a conclusion agreeable, he accepts it without argument, but
when he finds it disagreeable, he will bring against it all the forces
of logic and reason." Thucydides
The opposite is accepting good evidence or argument whether it suits us or not i.e. healthy scepticism.
I thank David Healy for coming to Australia in September of 2003. I listened to him speak about Let them Eat Prozac.
In
those two hours, all the organic, peculiar and undiagnosable
psychiatric presentations I had been seeing since recommencing work in
the public sector in 1997 after a three year break, suddenly made
sense.
I had one question to ask.
"David, has this passed any Daubert Hearings?"*
Professor Healy told me, "Yes six."
This
told me that the causal relationship of antidepressants to suicide was
scientifically sound, and that I needed to follow it up. And look at
the sublethal side effects all that led to suicide, psychosis,
hallucinations death wish, suicidal thinking, akathisia
*
The 1993 United States Supreme Court decision in Daubert v. Merrell Dow
Pharmaceuticals changed the criteria by which the views of experts are
to be admitted as scientific testimony in court.xvi
Daubert
was one of a thousand actions, on behalf of infants with abnormalities,
against the manufacturer of Bendectin, known in Australia as Debendox,
a common morning sickness remedy. The judges allowed evidence from
epidemiologists who had found no excess of foetal abnormalities among
the progeny of users of the drug. The judges barred from giving
evidence to a jury those experts who only pointed out that it was
impossible to prove that no causal relationship existed when Bendectin
use and foetal abnormality coincided.xvii
The
unanimous ruling states that the criterion of the scientific status of
a proposition is that is can be tested, particularly by way of a
logical process called ‘falsification’. That is, it must be possible to
specify a set of circumstances, the occurrence of which, would
demonstrate that the proposition is false.
In effect,
Daubert replaces the Frye and Bolam tests of ‘expert opinion’, being
that which is ‘generally accepted’ by a significant number of
authorities in the field, with Karl Popper’s notion of science as
‘knowledge’ which has withstood rigorous testing. This sometimes
entails a preliminary assessment, a Daubert Hearing, to decide if the
reasoning or methodology underlying the testimony is scientifically
valid.
Daubert has not been adopted in Australia where simple plausibility of expertise has held sway, with Adamcikxviii and Abalosxix
setting the standard. In each case, the High Court lost an opportunity
to comment on the difference between expert evidence within the
relevant body of scientific knowledge, and the unsupported opinions of
persons who held the status of being, professionally trained,
hence experts. The High Court, on each occasion, confirmed that
the judge or jury could choose whichever opinion they preferred.
Scientific
method includes putting up a proposition couched in the negative, a
null hypothesis, and testing it to see if it can be knocked down.
Examples of the null hypothesis are that the prisoner is not guilty and
that the unicorn does not exist. In junk science, the null hypothesis
is replaced by a positive assertion, one which cannot be proved to be
untrue even if it is untrue. One can never prove that a unicorn does
not exist, as it might always be just out of sight, so a proposition
asserting that a unicorn exists is not a suitable one for a scientific
investigation. The presumption of innocence is a null hypothesis, a
hallmark of good law as well as good science.
Although I was warned, by persons with experience, of what would happen to me
personally if I became involved in this issue, nothing, nothing could prepare
me for the Semmelweiss phenomenon, for bland denial by a vast number of my
psychiatric colleagues.
Yolande Lucire
www.lucire.com.au
lucire@ozemail.com.au
[i] Geddes J: Atypical antipsychotics in the treatment of Schizophrenia: a Systematic Overview and Meta-Regression Analysis BMJ.321 (2000)1371-1376
[ii] WhittakerRobert: Mad In America Perseus Publishing 2002.
[iii] Lillytrials.com
[iv] Harris G: Popular Drugs for Dementia Tied to Deaths. The New York Times, April 12, 2005
[v]
FDA Public Health Advisory: Deaths with Antipsychotics in Elderly
Patients with Behavioral Disturbances:
http://www.fda.gov/cder/drug/advisory/antipsychotics.htm
[vi] Meltzer HY et al.: Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial [see comment][erratum appears in Arch Gen Psychiatry.2003 Jul;60(7):735]. Archives of General Psychiatry, 2003. 60(1): p. 82-91.
[vii] Details from Professor C. Adams of the Cochrane Centre for Schizophrenia, Leeds, October 2004. Cited by David Healy.
[viii] Merson J: Epistemic Capture: The Science and Politics of Stress-related Illness. PhD thesis UNSW 2004.
[ix] Sachdev, P: Akathisia and Restless Legs. Cambridge University Press. 1996.
[x] Whittaker Robert: Mad In America. Perseus Publishing 2002.
[xi]
Philip Burgess, Jane Parkas, Damien Jolly, Harvey Whiteford, Shekhar
Sabena (2004) Do nations’ mental health policies, programs and
legislation influence their suicide rates? An ecological study of 100
countries
Australian and New Zealand Journal of Psychiatry 38 (11-12),
933–939 doi:10.1111/j.1440-1614.2004.01484.x
[xii] Press Release: Office of Elliot Spitzer May 13, 2004 http://www.oag.state.ny.us/press/2004/may/may13b_04.html http://www.centerwatch.com/patient/nmtresults/index.html
[xiii] http://www.fda.gov/cder/approval/index.htm
[xiv] Schulte J: Homicide and suicide associated with akathisia and haloperidol. American Journal of Forensic Psychiatry, 6:3-7, 1985.
[xv] Shear MK: Suicide Associated with Akathisia and Depot Fluphenazine Treatment. Journal of Clinical Psychopharmacology, 1983. 3: p. 235-236.
[xvi] Daubert v. Merrell Dow Pharmaceuticals Inc. 113 Supreme Court of the USA, 2786, June 28, 1993.
[xvii] Foster K.R. & Huber P.W: Judging Science: Scientific Knowledge and the Federal Courts, Cambridge Massachusetts: The MIT Press, 1997.
[xviii] Commissioner for Government Transport v. Adamcik (1961) 106 CLR 292.
[xix] Abalos v. Australian Postal Commission (1990) 171 CLR 167 F.C. 90/44.
 Back
to top Back
to top
|