|
Involuntary Commitment Alicia CurtisBad Subjects, Issue # 58 , December 2001
For those of us who work in the mental health system, and for those who live with a mental illness, our work and our lives intersect with the legal system around a complex and delicate decision. In certain situations, people with a mental illness can be made to go into a psychiatric hospital or institution against their will. This process is called an involuntary commitment and every state has a law for it, although those laws are not well known. In the state of Maine, where I live and work, this law means that if a person has a mental illness, and if they are in imminent danger of harming themselves or someone else, they can be put into a psychiatric hospital against their will. The police can initiate this process. They have the authority to take individuals into police custody if they have reason to believe the person has a mental illness and is at risk of substantial harm. Once the person is in custody, the police can then take them to the hospital for evaluation by a psychiatrist. If the psychiatrist believes this person to have a mental illness and to be in danger of imminent harm, the psychiatrist and another person fill out a certification of the need for involuntary commitment, which is also signed by a Justice of the Peace. This constitutes the initial involuntary commitment. The slang term for the certification process that is used by both workers and patients in the mental health community is "blue paper." The form authorizing the involuntary commitment is blue, and the phrase is used liberally as a verb: "Gee, I hope they don't blue paper me." Slang adds a touch of drollness to a controversial act that represents a difficult decision for doctors, as well as an often very upsetting process for the person being "blue-papered," and sometimes their family. (Although sometimes the family gets upset if the person is not blue-papered.) This initial blue paper holds the ill individual in the hospital for five working days. At the end of these five days, patients may sign in to the hospital on a voluntary basis or they may be discharged. Alternatively, if the psychiatrist feels that the patient continues to be an imminent risk of harm to themselves or others, and if the patient continues to refuse to stay in the hospital on a voluntary basis, there is another, more formal process of commitment which involves a court hearing before a judge. Many people outside of the mental health system are not necessarily aware of the law surrounding involuntary commitment. Yet most of the time those of us who work inside the mental health system take it for granted. I would like to step back from taking this law for granted and take a critical look at it. From a civil rights perspective, involuntary commitment creates a class of people who, at the discretion of a police officer, can be taken briefly into police custody and then placed in a sort of preventive detention. Patricia Deegan is an ex-patient and activist who refers to long stays in psychiatric institutions as incarceration, a word that is chosen for its political charge but I think also speaks to the lived experience of the patient. Involuntary incarceration clearly imposes a different standard of civil "liberty" onto the mentally ill than that which is theoretically guaranteed to the rest of us. If you are not classified as mentally ill, can you be confined somewhere for something people believe you are going to do, but which you have not yet done? Is there any evidence that persons with mental illness are actually more dangerous to others than random members of the general public? These questions are starting places for looking beyond common assumptions about role that involuntary incarceration plays in the interplay between civil rights and civil protections. For mental health professionals, the law can seem exceptionally frustrating when we are working with patients who are tormented and debilitated by their illness and unable or unwilling to receive treatment in the community. A patient who hears voices constantly, who exists in a state of fear about people she believes are trying to kill her, who does not take any medicines because she believes they are poisoned, and who is too distracted by her illness to cook meals or take showers, could probably not be committed to a hospital involuntarily. For those of us who entered a helping profession in order to help people who are suffering, this fact often feels like a tremendous failure of the system. Dr. Paul Chodoff, who has written several articles on the topic, points out that the focus of the involuntary commitment law on "imminent harm" as the main criterion for commitment, leads psychiatrists to feel frustrated that their work is aimed more at serving the police state in keeping dangerous people off the streets than in carrying out the aims of psychiatry. He argues that the involuntary commitment law should be broadened to allow commitment of those with a mental illness who need hospitalization due to the severe state of their illness, whether they are dangerous or not. The existing law about involuntary commitment is the result of a long dialectic between an attitude of paternalism toward the mentally ill and ideals of personal freedom and civil liberty. Both the state and the profession of psychiatry have evidenced paternalism towards those with a mental illness, which contrasts with constitutional rights that were revisited in the civil rights movements of the 1960s. Involuntary commitment has also been shaped by the history of psychiatry. The perceived need for involuntary hospitalization is a result of the way that psychiatric treatment was conceptualized and practiced in the nineteenth century. It also arises out of a social contract, wherein the State and the profession of psychiatry join forces to protect the public from a group of people who are seen as both terrifying and burdensome. The practice of involuntary commitment also arose as a result of the creation of the psychiatric institution as both the locus and the means for treatment of insanity. The institution was born of several different social forces. In early New England there had been a smattering of psychiatric hospitals, which had mostly started as single wards within general hospitals and had grown into separate buildings. Starting in 1810 there was a movement towards building psychiatric hospitals and institutions that continued to gather steam throughout the first half of the nineteenth century. This occurred in the context of overall changes in social welfare policy; there were new ideas and practices about the State being responsible for the indigent and the troubled, and other institutions for special populations such as the feeble-minded or epileptics were built at this time. The Victorian era brought a lower tolerance for disorder and deviance, and a sense of urgency about maintaining public safety and social order. At the same time there was a growing sense of idealism and excitement about the possibilities of a cure for mental illness. Whereas previous treatments for mental illness (exorcisms, bloodletting, emetics and purges) had generally not been successful and had contributed to a sense that insanity could only be subdued or confined, the new moral treatment being practiced in England promised the rehabilitation of the insane. 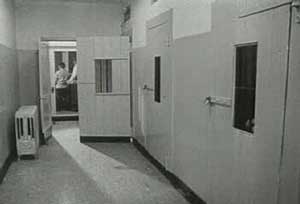 Maine's public psychiatric hospital was built in the
early nineteenth century to illustrate these new ideas and treatments. The
Maine Insane Hospital (often referred to at the time as the "Maine
Insane") was built in 1840 in Augusta, Maine. Governor Dunlop's speech
before the Maine Legislature in 1830, in which he advocated for the
creation of such an institution, clearly expressed the rhetoric of
collective social responsibility and hope for a cure: "Humanity loudly
calls for appropriate means of relieving and restoring to enjoyment and
usefulness"[those bereft of reason]"which means, are now not only beyond
the reach of the poor and friendless, but cannot be commanded by the
ordinary ability of our citizens or towns, on whom the duty of providing
for their support may fall." In keeping with the ideas of moral treatment,
the entire structure and experience of the hospital was designed as a kind
of treatment. The buildings and grounds represented a clean and orderly
environment which would restore the disordered mind to order. There was
proper ventilation to dissipate the bad vapors of insanity. Besides the
physical environment of the hospital, there was work, or occupational
therapy. The hospital was part of a 220 acre working farm, which
represented the key point of moral treatment. As the first report of the
hospital to the Maine legislature in 1841 stated: "Employment of some kind
is essential to the recovery of the insane. No employment is so congenial
to the human constitution as agriculture." Maine's public psychiatric hospital was built in the
early nineteenth century to illustrate these new ideas and treatments. The
Maine Insane Hospital (often referred to at the time as the "Maine
Insane") was built in 1840 in Augusta, Maine. Governor Dunlop's speech
before the Maine Legislature in 1830, in which he advocated for the
creation of such an institution, clearly expressed the rhetoric of
collective social responsibility and hope for a cure: "Humanity loudly
calls for appropriate means of relieving and restoring to enjoyment and
usefulness"[those bereft of reason]"which means, are now not only beyond
the reach of the poor and friendless, but cannot be commanded by the
ordinary ability of our citizens or towns, on whom the duty of providing
for their support may fall." In keeping with the ideas of moral treatment,
the entire structure and experience of the hospital was designed as a kind
of treatment. The buildings and grounds represented a clean and orderly
environment which would restore the disordered mind to order. There was
proper ventilation to dissipate the bad vapors of insanity. Besides the
physical environment of the hospital, there was work, or occupational
therapy. The hospital was part of a 220 acre working farm, which
represented the key point of moral treatment. As the first report of the
hospital to the Maine legislature in 1841 stated: "Employment of some kind
is essential to the recovery of the insane. No employment is so congenial
to the human constitution as agriculture." A hospital like this was seen as the means of treatment for insanity, and so the means of getting treatment was for the mentally ill to enter the hospital. The only problem was, how was it determined who needed treatment, and thus needed to be in the hospital? Psychiatry was a fairly young profession with few standard ideas about mental illness. Was it a disease of the organs and physical body like other diseases, or a disease of the humors and spirits? This was still a matter of debate. The only available basis for diagnosis was behavior, and for a young profession in a socially repressive age, the behaviors that supposedly expressed mental illness were often the same as the behaviors that expressed social aberrance, deviance, and "immorality." Many people were hospitalized with a diagnosis of "moral insanity." This concept may have been a precursor to the current diagnosis of antisocial personality disorder, but it also included such Victorian no-nos as masturbation and extramarital sex. There were also claims that husbands brought their wives to institutions just to be rid of them. The commitment law was created as a move toward reform. In 1874, Mrs. E.B.W. Packard, a one-woman whirlwind of a reform movement, successfully lobbied in the state of Maine for passage of a law to protect against wrongful commitment. She had been committed to an institution by her husband, a Calvinist minister, for arguing with him about Calvinist theology and feminism. Historians believe that Mrs. Packard probably did have a psychotic disorder, but that she would not need to be hospitalized according to modern standards. Before passage of the commitment law, in some states a husband could commit a wife to a psychiatric institution solely at the discretion of the superintendent of the institution. Mrs. Packard felt that a law creating a more formal process of commitment would bring order and justice to the system. In practice, though, people continued to be committed involuntarily for reasons having more to do with social control than psychiatric treatment. Husbands ridding themselves of wives via the psychiatric institution was still enough of a problem in the 1930s that the first woman in Maine's legislature, Gail Laughlin, authorized a bill penalizing husbands for bringing false testimony in the involuntary commitment hearings of their wives. I worked with a patient who in the 1960s had been brought to the hospital by her husband. The chief complaint listed on the admitting record was: "Patient does not do her housework." I think she did actually have a recurrent depression, a symptom of which was her inability to care for herself and her home, but there was obviously a large overlap conceptually between mental illness and not functioning in a proscribed social role. There is also a large history of the forced treatment of of homosexuality as mental "illness." One gay man I know has a familiar story. He was brought, as a teenager, to a psychiatric hospital in the Midwest by his parents, when they found out he had been having gay sex. He was involuntarily committed to the institution and treated for his homosexuality. (The treatment didn't work). Until the 1960s, the voice of paternalism asserted the need for involuntary commitment. But as African-Americans and women struggled for civil rights, there was renewed discussion and activism about civil rights for the mentally ill. Arguments for increased freedoms for the mentally ill took two paths, one somewhat fruitful and one less fruitful. Against the voice of paternalism, some people posed the radical question: Is there even such a thing as mental illness? For example, R.D. Laing made the famous argument that mental illness is a privileged state, an alternative viewpoint on the world. This argument at least challenged many assumptions of the mental health profession and caused them to be re-examined. On the other hand, the psychiatriast Dr. Thomas Szasz wrote a history of how early psychiatrists (such as Bleuler and Krepelin) created the diseases of mental illness by classifying certain behaviors that were disturbing to society in general, under the heading of a diagnosis, despite no evidence at the time of a cellular-level disease process. He viewed this process as the manufacture of disease, a sort of large-scale hoax which created and justified the social roles of psychiatrist and mental patient, and justified the practice of placing these patients against their will in a psychiatric institution. He regarded all of this as nothing more than a sanctioned form of social control. He saw a tacit contract existing between society as a whole and the class of psychiatrists, in which psychiatrists arrange to confine and control persons disturbing to society, in return for a social regard as members of the medical profession. Neither R.D. Laing's nor Thomas Szasz' arguments ultimately changed the laws and practices of institutions and involuntary commitment as much as did the arguments based on the principles of freedom and personal liberty intrinsic to America's self-definition. These arguments hold that despite the existence of mental illness, and despite the fact that the mentally ill might benefit from treatment, personal freedom is a higher order good than treatment. This focus on ideas of civil liberty coincided with a conceptual shift in the 1970s regarding the locus and modalities of treatment of mental illness. The institution had devolved from being a type of treatment to being a type of warehouse, and the community was seen as the best healing environment. Models of community-based treatment, like the community mental health center and assertive community treatment, also known as the ACT model, were developed. This change in thinking and practice shaped the current commitment law, which is based on the idea that someone cannot be detained or confined without extremely good cause. It also limits the duration of involuntary commitment, and ensures that no one individual or stakeholder may make commitment decisions. Currently dangerousness is the standard for commitment, as dangerousness is a relatively simple standard to define. But dangerousness is also a highly convenient standard, both because the criminal justice system already confines people who have been determined to be dangerous, and because of continuing public fears about the alleged dangerousness of those with a mental illness. This spring there was news in the New York Times that political dissidents in China were being forced into special psychiatric hospitals run by the police and given electro-shock therapy against their will. The mainstream organization of Chinese psychiatrist decried this practice. However this phenomenon makes obvious that wherever the mechanism of involuntary commitment exists, the possibility for abuse co-exists. It is still possible to distort the language and practice of psychiatry to overlap with social control. For instance a Chinese official discussed the idea of a political mania, the symptoms of which would be unreasonable suspicion, excessive and unhealthy energy directed in an obsessive manner to political organizing, despite the obvious negative social consequences of this activity. In any troubled relationship between the powerful and the less powerful, like the relationship between a repressive totalitarian government and a dissident citizen, or between parents and a gay teenager, or between husband and wife in a patriarchal society, the language and ideas of psychiatry and mental health practice are open to abuse as a form of social control. In these instances, the mechanism of involuntary commitment is also open to abuse as a way to confine those who are threatening to the social or political order. I therefore hope to see the practice of involuntary commitment continue to evolve as a balance between civil liberty and the need to care for those who cannot adequately address their own safety. I would not wish for the end of involuntary commitment, because I still view it as a way to provide treatment to those who refuse out of the fear, hopelessness, and suspicion that a mental illness can bring, and who might not otherwise survive. Alicia Curtis is a psychiatric social worker and a writer.
|
Copyright © 2001 by Alicia Curtis . All rights reserved.
Graphic: still image from Booked for Safekeeping,
taken from the Internet Moving Image Archive www.moviearchive.org.
Permission to link to this site is granted.