Current Research on Outpatient Commitment Laws
(“Laura’s Law” in California)

Jasenn Zaejian, Ph.D.
February 18, 2014
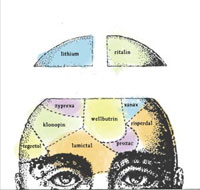
Outpatient commitment laws, passed by a number of states, permit forced commitment to treatment of those whom a psychiatrist, psychologist, or mental health official deems in need of treatment. The majority of this “treatment,” while not specifically stipulated in the law, results in coercive tactics to pressure agreement to take pharmaceutical preparations of limited-to-no effectiveness but – as shown in early research – with massive effects on cognitive functions and subsequent decision-making ability, not to mention a long-term or lifelong diminished quality of life and ability to function as a productive member of society.
Lately, however, research into the effectiveness of coercive treatment has been comparatively defunded, given the prevalence of pharmaceutical industry dominance in antipsychotic research. When such an approach is scientifically justified, that is one thing. Numerous research studies over the past 60 years have established that an enhanced voluntary services program for those diagnosed as “mentally ill” and incentive programs, including housing programs – are far more effective and consistent with social justice concerns than an involuntary commitment program, especially financial incentives used to gain cooperation by people with difficulty in functioning in society but resistant to current treatment.
New York State instituted an outpatient commitment law, “Kendra’s law,” about 15 years ago. While the NYS Office of Mental Health, in an assessment of the law’s effectiveness, specifies there is no racial disparity in its application, one only need look at the statistical database to see that there is certainly racial disparity. An analysis of NYC’s outpatient commitments by Kendra’s law between 1999-2010, presented in the following table, clearly indicates prima facie racial discrimination:
Racial Characteristics From NYC Census
NYC Pop. Census Kendra NYC Commitment
African Am. 15.9% 36%
Latino(a) 17.6% 38%
Asian 12.7% 3%
White 65.7% 23%
In California, the Orange County Board of Supervisors are now preparing to adopt “Laura’s Law,” identical to New York’s Kendra’s law in its emphasis on legal outpatient commitment. The Board of Supervisors have been presented with research data clearly indicating that legal forced commitment to treatment is less effective than voluntary enhanced treatment.
The Psychiatric Rehabilitation Association has repeatedly stated its strong opposition to involuntary outpatient commitment as presented in the association’s recent 2013 statement:
“Recovery is possible when the individual in treatment acts in partnership with the rehabilitation workforce and strengthens integration into their community; coercion is not an incentive to recover and all too frequently may be implemented where other treatment and community support options could achieve a better result.”
However, most recently following the reaction to the Orange County press coverage of the killing of a “mentally ill” individual who was beaten to death by police (currently under review by the US Dept. of Justice), the false conflation of violence and mental illness has reemerged, resulting in legislative officials ignoring the worldwide research on the ineffectiveness of outpatient involuntary commitment when compared to the effectiveness of increased funding for enhanced voluntary mental health services. The real problem in the killing was the ineffective training of the police in dealing with a supposedly “mentally ill” individual, who was sitting at a bus stop when confronted and repeatedly stated he was doing nothing wrong. He was badly beaten and died of his injuries.
What would likely have saved him is a liaison with the Fullerton Police of a local mental health agency clinical staff person, on call for every encounter with a potentially “mentally ill” individual. We had this in the 70’s when I worked as a young clinical psychology post-doc intern at a California Community Mental Health Clinic. I recall going out in the middle of the night with Sheriff’s deputies. In other major metropolitan areas, I subsequently participated in training sessions with SWAT team members and other police on how to relate to a disturbed person. One has to wonder what happened to this system. A legal outpatient commitment would not have saved this person from being beaten to death, yet the public and the Board of Supervisors are supporting outpatient commitment as a reaction, not based on reason but on the public’s unwarranted fears and basic ignorance of those who are diagnosed as mentally ill.
Parents dealing with disturbed young adults, as well as parents’ groups, embrace the false belief that a legal outpatient commitment to treatment will provide a solution. This is compounded by the well-funded and nationally organized distortions of research presented by the Treatment Advocacy Center (TAC), an organization created after the National Alliance for the Mentally Ill (NAMI), posing as a parent advocate group, was discovered by Senator Grassley’s group and investigative reporters to be covertly funded by the pharmaceutical industry. TAC was formed by a former NAMI creator and his associate from the advertising industry. This action served to distance themselves from NAMI. Both groups have distorted and denied significant research that disagreed with their opinions. TAC is funded by a corporation that engages in pharmaceutical research, the Stanley Foundation. Soon after TAC’s formation, the former advertising industry person reportedly suggested they falsely conflate mental illness with violence to elevate the public fears so that laws will be passed to promote their views and manipulate the mental health industry, state, and local governments to succumb to their unscientific beliefs. The ultimate, transparent goal of their strategy is to legally force all whom they deem in need, into pharmaceutical treatment.
Sound research repeatedly proves most of their assumptions, beliefs, and proclamations are in serious error. Yet their target audience is the general public, for purposes of generating fear. The public does not necessarily follow the scientific research on these issues. Not many citizens are aware of the serious detriments to an individual’s mental health, physical health, and the financial implications of implementing a law requiring involuntary commitment. If such a law proved scientifically valid, the effort might be justified. But studies, including those reviewed by the Rand Corp, cited below, proves that it has little if any scientific support. In fact, a far less expensive enhanced voluntary services program has proven, in numerous international studies, to be far more effective.
California counties with large populations will incur significant unanticipated court and legal costs if they implement the law. In Orange County, south of Los Angeles, the county behavioral health director who is reportedly in support of implementing the law, recently indicated in the press that it would apply to “120” clients. While the state will provide some funds if the county implements the law, the costs for those 120 could well exceed $50 Million to the county, over what will be provided from the state, including court operating costs, attorney fees, salaries for involved police and sheriff deputies, salaries for mental health officials involved, state mandated enhanced services, and oversight. The conclusion of the recent Rand Corp. study on the matter, updated November, 2012 is quoted here:
“A RAND team led by Susan Ridgely reviewed the available studies, interviewed stakeholders in eight states, and analyzed administrative data on services provided by California’s county mental health contract agencies. Their conclusion:
• There is no evidence that a court order is necessary to achieve compliance and good outcomes, or that a court order, in and of itself, has any independent effect on outcomes.”
A far egregious matter involves how the law is applied. Martin Luther King’s dream of a post-racial America has not been achieved, regardless of popular rhetoric. This fact is clearly reflected in the racial disparity in our major institutions, corrections, and mental health. Significant evidence that the local, state, county, and federal mental health systems and agencies are racially biased – albeit subtly – is denied in most cases. Since at least the 1960’s diagnostic research has demonstrated a racial bias in psychiatric diagnosing, where major mental illnesses are over-diagnosed in ethnic populations. Much of this is swept under the rug.
In the 1980’s, a colleague, preferring anonymity, who had previously worked as a tenured university professor teaching experimental psychology, took a job as a program evaluation director in a major California psychiatric hospital. His position included publishing studies. One such study he was about to publish established a statistically significant racial bias in discharge planning of African Americans and Mexican-Americans who identified with their Mexican culture. Administrators threatened him with a search warrant of his private residence if he did not produce all copies of the original data of the study. He was eventually removed from his position and forced out of the job (personal communication).
Within the past decade before retiring, prompted by curiosity why the hospitalized population represented a far greater proportion of African Americans, I completed an informal study of race-based diagnoses at a major metropolitan forensic hospital where I held the title of director of program evaluation. An African-American, Haitian-American or other black person on admission had (if memory serves) a 70% chance of receiving a schizophrenia diagnosis compared to less than a 50% chance of a white person or Asian person walking through the door. Odds for a Latino of a schizophrenia diagnosis was around 60%. Many formal studies confirmed similar racial disparities.
The psychiatrist and scholar Jonathan Metzl, in his 2010 book The Protest Psychosis presents confirming data that the diagnosis of schizophrenia has become racialized, a “black disease,” as many activists and civil rights protestors have fallen under the eye of the mostly white psychiatric system run by white-privileged psychiatrists, psychologists, and other white mental health professionals. Experience as well as research informs us that people of different ethnicities who present anger and opposition at being institutionalized or forced to be evaluated by white professionals or ethnic professionals identifying with the white mainstream are labeled with one of the variants of “schizophrenia,” most commonly paranoid schizophrenia.
How does this racial diagnostic disparity bear on the implementation of an outpatient commitment law in California, or any other state for that matter? One need only look above at the NYC statistics on racial disparity in the implementation of Kendra’s law to see how it will apply if Laura’s law is implemented. Based on solid research over the past 15 years of similar laws, it is anticipated that the implementation of Laura’s law will result in racial disparities, opening Orange County and other California counties once again to civil rights lawsuits, judgments, and other unanticipated expense to taxpayers but negative – if any – benefit to the people who happen to fit the criteria for legal outpatient commitment. A criteria, based on opinion, not sound science.
In reviewing the world’s history of treatment of mental difficulties, one can discover numerous instances of effective creative approaches. All states, including California, need an enhanced mental health program that transcends the rigidly uncreative mainstream operation that it now is, not another law based on a knee jerk reaction as was done with New York’s Kendra’s Law. As a result on the law becoming institutionalized, NYS Mental Health officials continue a strategy to obfuscate its true ineffectiveness: an oppressive law that is based on opinion, naiveté, knowledge deficits, and ignorance of what really does work, while ignoring more than 60 years of worldwide research that mostly opposes it. The people of California need a mental health system, reorganized in a creative fashion, utilizing positive and relevant contingency management or motivational incentives to encourage those reluctant to accept involvement to attend voluntary programs. They certainly do not need another law that harms the public welfare, benefitting political agendas while creating more pain, suffering, and alienation for those in our society who are most needy.
 Jasenn Zaejian, Ph.D.
Jasenn Zaejian, Ph.D.Following a 33+ year career as a clinical psychologist, neuropsychologist/researcher, psychotherapist, psychology department director and clinical supervisor, psychiatric hospital middle manager and program evaluation director at a major metropolitan psychiatric hospital, Dr. Zaejian retired to devote his energies to writing critical psychology and self help books. Healing Personal Psychology, a critique of main stream psychology, was published in 2011. Healing Personal Depression was published in 2012.








Treatment can be enforced through judicial order only in those patients that have multiple admissions due to non-compliance with treatment and/or are deemed to be dangerous to themselves and/or others.
Blacks and Latinos in NYC constitute the bulk of mandated treatments because they are the groups that due to economical limitations receive the least support from the community to adhere to treatment.
@ mah3md,
Adherence?
Adherence to *what*?
Why should someone be forced to *adhere* to anything remotely similar to mind-altering drugs that cause injury under the guise of “treatment?”
If someone is deemed to be dangerous, then the psychiatric community needs to PROVE IT.
In court; a real court, with appropriate legal counsel for the person being charged with the “crime” of emotional distress.
For the sake of accuracy, can you docs please stop calling forceful drugging of a fellow human beings “treatment?”
Those fellow human beings, with human rights also happen also to be fellow *citizens* – with constitutional rights, which are guaranteed in the 1st, 8th and 14th amendments.
http://psychrights.org/articles/rightorefuse.htm
Your comment about Blacks and Latinos… Let me get this straight: “Economic limitations and lack of community support” are the reasons these groups don’t adhere? You lost me there. Emotional distress is treated as a crime, and these groups are targeted. because they are often without the financial means and education to fight the system we have in place. That’s how I see it.
Duane
Thank God for this attorney:
http://www.madinamerica.com/2014/02/psychrights-ask-supreme-court-hear-appeal-alaska-supreme-courts-daniel-g-decision/
Duane
Duane
Great response. Thank you.
Stephen,
I’m grateful for your presence on this site, and for your heartfelt comments – every time I log on to read.
Duane
Mr. Duane, Sir:
Please read again my posting and respond to the positions I presented. Solipsistic thoughts do not carry any weight.
I did not say, or even implied, that the so-called minority groups do not adhere to psychiatric treatments “due” to lack of support but “because” of lack of support in the community. “Non-adherence” is not only with Psychiatry treatments in particular but with Medical treatments in general and thus not adhering to different treatments: Cardiovascular (like hypertension and cholesterol control,) Metabolic (diabetes, obesity) Eye and Ear (glaucoma, retinopathies, decreased hearing,) Gastroenterological (from perforated duodenal ulcers to bleeding hemorroids,) Infections (from complex dermatological suppurative lesions to HIV advancing into AIDS) and so on and so forth. These minorities that refuse every kind of treatment have shortened life spans and, goes without saying, constitute the majority of the homeless and street people that present with severe untreated illnesses, both mental and physical (a silly difference but that is vastly used) and populate the emergency rooms. The “right” to refuse treatment should not stop with Psychiatric treatments but with ALL treatments. Is it not true?
There is no question that everybody, patients or not, must be protected in their rights and nobody denies that. You do not need to quote every Constitutional amendment to support this notion. But as important as the protection to refuse treatment is so is the right to be treated and when a person lacks the ability to understand this need then the society must intervene to facilitate treatment, at times above the wishes of the patient. Mentally ill patients can certainly be dangerous TO THEMSELVES, and they are unable, in many cases, of controlling their impulses and their lack of insight supersedes rationality and that that takes them to refuse treatment and therefore put themselves in a vulnerable state. To obtain a permission to treat above… read more
Mr. Duane, Sir:
CollapsePlease read again my posting and respond to the positions I presented. Solipsistic thoughts do not carry any weight.
I did not say, or even implied, that the so-called minority groups do not adhere to psychiatric treatments “due” to lack of support but “because” of lack of support in the community. “Non-adherence” is not only with Psychiatry treatments in particular but with Medical treatments in general and thus not adhering to different treatments: Cardiovascular (like hypertension and cholesterol control,) Metabolic (diabetes, obesity) Eye and Ear (glaucoma, retinopathies, decreased hearing,) Gastroenterological (from perforated duodenal ulcers to bleeding hemorroids,) Infections (from complex dermatological suppurative lesions to HIV advancing into AIDS) and so on and so forth. These minorities that refuse every kind of treatment have shortened life spans and, goes without saying, constitute the majority of the homeless and street people that present with severe untreated illnesses, both mental and physical (a silly difference but that is vastly used) and populate the emergency rooms. The “right” to refuse treatment should not stop with Psychiatric treatments but with ALL treatments. Is it not true?
There is no question that everybody, patients or not, must be protected in their rights and nobody denies that. You do not need to quote every Constitutional amendment to support this notion. But as important as the protection to refuse treatment is so is the right to be treated and when a person lacks the ability to understand this need then the society must intervene to facilitate treatment, at times above the wishes of the patient. Mentally ill patients can certainly be dangerous TO THEMSELVES, and they are unable, in many cases, of controlling their impulses and their lack of insight supersedes rationality and that that takes them to refuse treatment and therefore put themselves in a vulnerable state. To obtain a permission to treat above objections under the AOT guidelines (Kendra’s Law) a lawyer is assigned to the patient to defend his/her right to refuse treatment, the Psychiatrist presents the case and requests treatment over objections based on three main instances: Dangerous to self, dangerous to others, inability to care for self. A judge weights the arguments and issues a decision. Yes, to obtain an order of treatment over objections the Psychiatrist must PROVE in court any or all of the above mentioned three instances.
You should witness these court procedures and see how many times the Psychiatrist fails to PROVE his/her case for treatment over objections and the request is denied.
I agree that the rights protected by the Constitution applies to the mentally ill and should be defended, including the right to vote and to redress grievances in court, like refusing treatment. But then the resulting questions are:
- Should we defend the right to own a gun for protection under the second amendment as the NRA interprets it or, as the NRA states, we should deny it to people with mental illness.
- If a mentally ill person commits a crime, should we do away with the M’Naughten rule (ability to tell right from wrong)? Well, if the patient refused treatment and the society does not consider him mentally ill and he is considered able to refuse treatment then the society can refuse to consider that any crime he commits in the absence of treatment has been done with total free will and years of legal proceedings that protect the mentally ill will be trashed.
- If the patient can refuse psychotropics, so can the Psychiatrist refuse to administer them without fear that the results of The Osheroff vs Chestnut Lodge case applies to him/her?
- If a Psychiatrist learns of the threat on somebody’s life verbally made by a patient under his/her care, should the therapist forsake warning the potential victim, without suffering consequences from cases like the Tarasoff vs Regents of University of California because the patient is exercising unimpeded free will and you are violating the patient’s rights to conduct treatment and to privacy?
These arguments, directly or indirectly related to the right to refuse treatment, can be even more complex and extend forever and cannot be encapsulated in ideological bromides.
Finally, let me say that the implications of “racism” of the AOT program are totally false. The program was based on the outrage generated by one very white paranoid schizophrenic that, having refused treatment and following command hallucinations, pushed a very white person into the path of the subway, producing the death of the person.
Are there psychiatric abuses being committed? Yes. Should we ignore them? No. Does this mean that all of Psychiatry is abusive and should be dismissed? Absolutely not, but Psychiatry has to be corrected, not eliminated.
Forums like this one are good to discuss issues, but people should not argue with vacuous diatribes and set forth arguments based on what one thinks has been said and not to what was actually postulated. This distortion of thought belongs to the Beck/Limbaugh School of Willful Distortions and not to what should be a civilized exchange of ideas.
I do not think that I am correct in every aspect that I present and I find that starting a polemic in sites like this could be useful to develop common understandings. As it stands, pseudo-arguments do not protect psychiatric patients but make them more vulnerable.
@ mah3md,
You wrote:
“You do not need to quote every Constitutional amendment to support this notion.”
I did not quote *every* amendment, I referred to three: 1st, 8th and 14th.
They are routinely *ignored* by the psychiatric community.
You wrote:
“These minorities that refuse every kind of treatment have shortened life spans and, goes without saying, constitute the majority of the homeless and street people that present with severe untreated illnesses, both mental and physical (a silly difference but that is vastly used) and populate the emergency rooms.”
It’s hard to know where to start. I suppose a good place would be that health treatment for medical illness is nothing like “treatment” for mental illness. I would simply ask you: If an adult refuses conventional cancer treatment, do the authorities show up? Is he/she forced to undergo chemotherapy, radiation, etc? I say that if an individual cannot decide what medical treatments to say ‘yes’ or ‘not to… what rights do they have left?
The 2nd amendment… States have historically been able to make these decisions when it comes to someone with a “history of mental illness” -
http://www.ncsl.org/research/civil-and-criminal-justice/possession-of-a-firearm-by-the-mentally-ill.aspx
IMO, there ought to be a process by which a psychiatric diagnosis can be *removed* -
http://psychdiagnosis.weebly.com/
Also, if a person has no history of violence, and has fully recovered from a “psychosis” – especially one that was prescription-drug induced. -
http://www.madinamerica.com/2011/11/bipolar-illness/
They should have recourse to the state where they reside. Also, veterans who have taken an oath to “support and defend the Constitution of the United States… should not arbitrarily lose their 2nd amendment rights for being treated for PTSD.
The 2nd amendment topic would probably be best debated on the *new* MIA forum, ‘All Things Political: Thoughts on a Paradigm Shift – from the Left, Right and Center’. This would be an ideal… read more
@ mah3md,
You wrote:
“You do not need to quote every Constitutional amendment to support this notion.”
I did not quote *every* amendment, I referred to three: 1st, 8th and 14th.
They are routinely *ignored* by the psychiatric community.
You wrote:
“These minorities that refuse every kind of treatment have shortened life spans and, goes without saying, constitute the majority of the homeless and street people that present with severe untreated illnesses, both mental and physical (a silly difference but that is vastly used) and populate the emergency rooms.”
It’s hard to know where to start. I suppose a good place would be that health treatment for medical illness is nothing like “treatment” for mental illness. I would simply ask you: If an adult refuses conventional cancer treatment, do the authorities show up? Is he/she forced to undergo chemotherapy, radiation, etc? I say that if an individual cannot decide what medical treatments to say ‘yes’ or ‘not to… what rights do they have left?
The 2nd amendment… States have historically been able to make these decisions when it comes to someone with a “history of mental illness” -
http://www.ncsl.org/research/civil-and-criminal-justice/possession-of-a-firearm-by-the-mentally-ill.aspx
IMO, there ought to be a process by which a psychiatric diagnosis can be *removed* -
http://psychdiagnosis.weebly.com/
Also, if a person has no history of violence, and has fully recovered from a “psychosis” – especially one that was prescription-drug induced. -
http://www.madinamerica.com/2011/11/bipolar-illness/
They should have recourse to the state where they reside. Also, veterans who have taken an oath to “support and defend the Constitution of the United States… should not arbitrarily lose their 2nd amendment rights for being treated for PTSD.
The 2nd amendment topic would probably be best debated on the *new* MIA forum, ‘All Things Political: Thoughts on a Paradigm Shift – from the Left, Right and Center’. This would be an ideal place for you to trash Limbaugh/Beck if you feel the urge to do so.
My *politics* are best found here:
http://archives.gov/exhibits/charters/
… Oh, that pesky Constitution… those nasty conservatives and libertarians.
Well, we’re not going away in this fight. We’re going to join hands with those on the center, and those on the left, until we get this job done. Get used to us.
Duane
CollapseThe *new forum*. ‘All Things Political’ can be found here:
http://www.madinamerica.com/forums/
Simply start a ‘new topic’ in this section, if interested.
IMO, this would be the place to have a healthy debate on 2nd amendment rights (rather than detract from the original topic of the blog author’s post).
Duane
Comment removed.
Doc,
You accused me of expressing “solipsistic thoughts”.
Rather harsh statement, don’t you think?
Duane
I have seen many of the above, mostly in white European form make complete recovery and return to normal taxpaying status through non drug, independent self help groups.
mah3md,
I don’t usually post at MIA anymore but you’ve made a few comments here that I feel the need to address.
First, Andrew Goldstein (whose murder of Kendra Webdale became the impetus for Kendra’s Law) did most certainly *NOT* refuse treatment and you are libelling him when you say that he did. Mr. Goldstein knew he was in serious trouble, requested mental health care and was turned away repeatedly. This tragedy represents another failure of our *voluntary* system. What should have happened is increased access to uncoerced mental health care but instead it became further encouragement for the forced drugging enthusiasts.
We don’t have enough resources for those who want help because we’re too busy forcing it upon people who don’t. In my own case, three years ago, I was extremely psychotic and manic. We went to the emergency room many, many times and I was turned away as having “borderline personality disorder,” i.e. couldn’t be helped. My mother was told to stop “enabling” me by bringing me to the hospital. As I got sicker and sicker, my behaviour became more and more bizarre. Eventually, I broke the law, stood trial, was convicted, and one of the terms of my probation was to receive mental health care (Yes! The very same mental health care that I had been requesting.) So, mah3md, would you characterize me as one of those patients lacking in insight and requiring forced treatment?
Secondly, you confidently state that a patient’s illness can make him refuse treatment. But the only evidence you’ve got for this is that he’s refusing treatment. What about those who refuse psych treatment for good medical reason, e.g. that they do much better without it? The trouble is that the only test we have for lack of insight is disagreeing with the mental health system.
So Kendra’s Law isn’t racist, it’s classist? For Heaven’s sake…
Cataract,
Good point.
I hope we can one day move beyond *both* racism and classism. My wife of 24 years, happens to be Latina. I don’t consider her to be in a different *class*. In hindsight, I should have simply said *some people* do not have the resources to fight the psychiatric establishment.
Duane
Comment removed for infringement of posting guidelines.
The paradox of AOT is that individuals who actively seek treatment can rarely access that treatment which makes a difference. An ever growing population of individuals on disability by virtue of mental illnesses evidences this stark reality. AOT is only treatment when treatment is both everything and nothing and individual rights, goals, needs, and dignity mean little.
I fear an “enhanced mental health program” in deed is wishful thinking. (We all remember the optimism subsequent to the passage of Proposition 63 in 2004.) Where there seems nary a program that doesn’t represent a comprehensive array of services and supports under the rubric of Wellness & Recovery the words and deeds fail to intersect. Instead we often see a system that evidences the united opinion of the President Bush’s New Freedom Commission on Mental Health “in shambles.”
For Parents
As a ‘young person’ in 1980 I voluntarily asked for talking therapy, declining medication. I was given Modecate depot. Modecate Depot disabled me and triggered a number of suicide attempts. These Control Drugs are dangerous and cause homicides.
(In 1984 I quit depot, I asked for milder oral meds and slowly tapered, and with psychotherapy made complete recovery).
The other ‘young people’ in hospital with me at the time remain either disabled or are dead.
Adolescent Psychiatric Hospitalization and Mortality, Distress Levels, and Educational Attainment, Follow-up After 11 and 20 Years at http://archpedi.jamanetwork.com/article.aspx?articleid=485793