ANCHORAGE — Two courtrooms, two floors of the Nesbett Courthouse, two views of Zyprexa.
In Courtroom 403, lawyers read corporate memorandums to a jury that must decide a lawsuit brought by the state of Alaska, which claims that the drug maker Eli Lilly hid the dangers of Zyprexa, Lilly’s best-selling schizophrenia medicine.
At the same time, in Courtroom 301, William Bigley had his own opinions on Zyprexa, and all the other drugs he has taken since 1980 to battle demons that only he can see. On this day, March 14, a state court judge would decide whether Mr. Bigley should be held for 30 days in a psychiatric hospital.
Mr. Bigley, 55, told the judge that the drugs were “poison” and that he did not need them. “I’m fine,” he said. His words were sadly undercut by his regular pronouncements that he knows President Bush, owns a private jet and has seen flying saucers. Of all the facts at issue in the two courtrooms, one is beyond debate. Mr. Bigley is not fine.
Even so, Mr. Bigley’s hearing — which had an unexpected outcome — offered a textbook illustration of the agonizing choices faced by mentally ill patients as they consider taking Zyprexa and similar medicines, called antipsychotics.
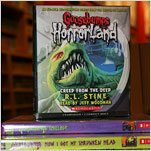
By calming the hallucinations and delusions that plague people with schizophrenia, drugs like Zyprexa allow many patients to live outside psychiatric institutions.
But the documents being discussed in Room 403 offered plenty of evidence that Mr. Bigley, whatever his delusions, has good reason to dislike the medicines.
All antipsychotics have side effects, and Zyprexa’s are among the worst, according to the American Diabetes Association and independent scientists. In many patients, Zyprexa causes severe weight gain that can lead to diabetes, as well as sharply higher cholesterol and triglyceride levels in the blood. Those are all risk factors for heart disease, the leading killer in the United States.
Further, the documents introduced in Courtroom 403 show that for much of the last decade, Lilly executives played down those risks. Among themselves, in internal e-mail messages and memorandums, they shared worries that Zyprexa’s sales would fall if the drug was linked to weight gain or diabetes.
In 2002, for example, the Japanese government ordered Lilly to warn Japanese doctors against giving Zyprexa to people at high risk for diabetes. But Lilly did not add a similar warning to Zyprexa’s label in the United States. Internally, Lilly executives acknowledged that the warning had hurt Zyprexa sales in Japan.
“The impact of the label change in Japan has been very profound,” two senior Lilly executives wrote in a memorandum on July 1, 2002. “There has been a 75% drop in new patients who are being put on the drug.”
Indeed, as American doctors have learned on their own about the connection between Zyprexa and diabetes, prescriptions for Zyprexa have plunged. Since 2003, they have slid 50 percent.
Yet Zyprexa, which sometimes works better than other antipsychotics on severely ill patients, remains widely used. In the United States, it is still prescribed almost four million times a year. It had sales worldwide of $4.8 billion in 2007, half in the United States.
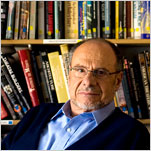
Mr. Bigley’s case illustrates why psychiatrists and patients feel they have no choice but to use Zyprexa, whatever its side effects. Mr. Bigley, a thin man with greasy black hair, cloudy eyes and a salt-and-pepper beard, has been hospitalized more than 70 times since his first breakdown in 1980.
Psychiatrists say he has paranoid schizophrenia with symptoms of mania. Over the years, he has been medicated with Zyprexa, Risperdal, Haldol, Thorazine and many other psychiatric drugs, despite his objections.
Exactly how many times Mr. Bigley has been put on Zyprexa over the years is unclear. But medical records from his hospitalization in December 2006 refer to his complaints that Zyprexa was making him hungry — a common side effect. Psychiatrists took him off Zyprexa and gave him Seroquel, another antipsychotic, in its place.
In 1999, a judge found him incompetent to care for himself and appointed a guardian to oversee his affairs.
The records also show that neither Zyprexa nor any other drug has given Mr. Bigley any lasting relief, and that he always stops taking his medicines after being released from the hospital. Unmedicated, Mr. Bigley is jittery and quick to anger. In conversations with a reporter, he was nearly incomprehensible, spewing complaints and curses about the way he is treated.
But Mr. Bigley has never been known to be violent or suicidal. Despite his psychosis, he has survived Alaska’s harsh winters. He bounces among apartments, group homes and the Alaska Psychiatric Institute, the state-run mental hospital in Anchorage, mumbling about the Secret Service and other favorite topics to anyone who will listen.
But he makes one point with absolute clarity: He does not want to be medicated or hospitalized.
On March 14, he repeated that request to state court Judge Jack W. Smith, who was hearing the psychiatric institute’s request to confine him.
There was little reason to believe that Judge Smith would side with Mr. Bigley. Hearings like his usually last only a few minutes. Psychiatrists and advocates for the mentally ill say that judges prefer not to second-guess doctors and typically rubber-stamp the requests of hospitals to confine and medicate patients.
As he sat before Judge Smith, Mr. Bigley — who had asked that his hearing be open to the public — hardly seemed like a good candidate for release. He fidgeted and interrupted the proceedings as his lawyers shushed him. He had been brought to the Alaska Psychiatric Institute on Feb. 23, after squabbling with housemates at his group home, where a resident called the police.
Dr. John Raasoch, a doctor at the hospital who treated Mr. Bigley, said that Mr. Bigley had irritated the staff and other patients.
“He’s yelling, swearing on the unit, he hit the door,” Dr. Raasoch said. Antipsychotic medication would calm Mr. Bigley and make him more cooperative, the doctor said.
“There’s no point to have a psychotic individual in the hospital and not be able to treat him,” he said. “I think he’s suffering severe distress.”
But Judge Smith appeared worried about both the side effects of antipsychotic medicines and that Mr. Bigley’s history suggested he would not benefit from them.
“We’re getting a short-term fix that doesn’t change Mr. Bigley’s underlying condition,” he said.
Under Alaskan law, a person cannot be forced to take medicine against his will simply because a psychiatrist says he is unhappy or delusional. Mr. Bigley could be confined and medicated only if Judge Smith found he was violent, suicidal or a grave danger to himself because of his mental incompetence.
Mr. Bigley was not violent or suicidal, Dr. Raasoch said. But the doctor said he was in grave danger because he might irritate other people, including police officers, to the point where he might end up being hurt.
“He’s very inappropriate,” Dr. Raasoch said. “He gets up in people’s faces. I think the majority of people would just punch him.”
Elizabeth Brennan, the public defender representing Mr. Bigley, agreed that Mr. Bigley can be difficult. But Mr. Bigley is not in grave danger simply because he is a nuisance, and confining and medicating him would not help him, she said.
“The hospital has not shown that treatment will improve him,” she said.
After nearly an hour of testimony, mainly from Dr. Raasoch, Judge Smith appeared troubled by the thought of confining or medicating Mr. Bigley against his will.
“It sounds like aside from getting in and out of the hospital, he gets by,” the judge said. “That’s a choice that he should be allowed to make.”
And so Judge Smith ordered the hospital to release Mr. Bigley, though he acknowledged that Mr. Bigley was likely to be picked up again in a few weeks, or months at most.
“I don’t find by clear and convincing evidence he’s gravely disabled,” Judge Smith said.
Though the decision was unusual in such cases, Mr. Bigley did not seem overly surprised, or even pleased.
“There’s nothing wrong with my head in the first place,” he said to the judge, inserting a seven-letter epithet. Within a few seconds, he began to hector Steve Young, his state-appointed guardian, demanding that he be given a hotel suite. “He’s going to give me a dirty place,” Mr. Bigley complained.
With that thought, Mr. Bigley headed for the street, his brain in chaos but his body free from the side effects of the medicines he will not take. One floor up, lawyers for Lilly and the state argued on, debating whether Zyprexa’s benefits outweighed its risks — a choice Mr. Bigley, sound mind or not, had already made.